The NCIN (National Cancer Intelligence Network) is a UK-wide initiative, working to drive improvements in standards of cancer care and clinical outcomes by improving and using the information collected about cancer patients for analysis, publication and research.
When I was first aware of the NCIN, their goal was “To develop the best cancer information service of any large country in the world – by 2012”.
Because of the work they continue to do, UK clinicians, medics, researchers, NHS purse holders, pharma, charities and, of course, patients are now able to draw on an incredible amount of useful data-sets. This data enables measures to improve outcomes, drug development, research projects, awareness and own patient care.
This year I was honoured to be invited again to attend the NCIN Conference with a bursary place and below is a summary from my notes at the Conference. Wherever available I have added links to presentations.
Cancer Outcomes Conference 2014 – the power of information
Sponsored by Cancer Research UK and Macmillan
Chris Carrigan
Director of NCIN Public Health England (PHE)
Chris opened the conference and welcomed those attending. This year’s conference attendance is larger than ever before with over 570 people attending. With national and international spread from primary to end of life, charities and patients.
Chris (@C_Carrigan) wrote a blog at the start of the conference on twitter on how bringing people together can improve cancer outcomes – read here
Harnessing the power of information to deliver quality and innovation in cancer surveillance, services and outcomes
Chair: Prof Brian Ferguson
Knowledge Transfer and Innovation Director at PHE
“Innovation at the heart of Public Health England.
Kris Hallenga
Coppafeel! @krispop @coppafeelpeople
Ensuring everyone stands the best chance of surviving breast cancer
Kris ‘story’ is well documented not least on an incredible documentary that has just been shown on TV “Dying to Live“.
Kris was 22 when she noticed lump. She ignored for a long time. Eventually went to GP and told more likely to be hormonal. Went travelling and noticed the lump was getting bigger. Returned to GP. Told nothing. Mum got involved. Returned to GP. 8 months after first going to GP was referred and told breast cancer and spread to spine.
1 in 15,000 chance of getting breast cancer under 25.
“You beat the odds in getting the disease and can beat the odds to get rid of cancer.”
2 months into treatment Kris researched why she didn’t know more about cancer at a younger age and what to expect.
She knew she couldn’t change her diagnosis but she could make it better. Or as Kris said “You can’t polish a turd… but you can roll it in glitter…”
She kept hearing “Early detection is the best form of defence.” Why wasn’t there breast cancer awareness in schools, universities, 6th form colleges? Surely that’d lead to earlier detection.
So Kris thought about where she could reach these young people. Armed with CoppaFeel! stickers set off to a festival. Whilst facepainting with her twin sister people started approaching and talking about boobs. Talking about breast cancer. Talking about checking yourself.
CoppaFeel! are now a regular set up at music festivals, university campus and many other locations filled with younger people.
As well as Kris and her sister talking about boobs, there are now the Boobettes – young women who’ve been diagnosed with Breast Cancer. They go into and talk at schools and events about their experiences and awareness and early diagnosis.
Kris has asked “What does BC mean to young people?” and got these answers (amongst others) – life-stopping, turmoil, depressing, threatening, damaging… not good and words that put you off from checking your boobs.
It is a very treatable disease if diagnosed early.
1 in 3 are diagnosed with cancer. Early diagnosis is key. #rethinkcancer is a campaign to bring cancer education into schools, colleges and universities. “I know it will help and I know they want to know it… I’ve spent the last 5 years speaking with them.”
Put an end to late diagnosis of cancer.
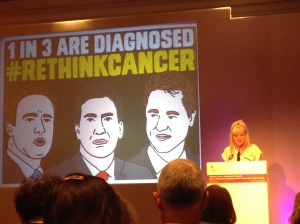
The stats of tomorrow are the young people of today… it can happen to young people. It should go through the mind or every GP and medical professional out there.
“If you have influence please use it. If you have colleagues please pass the message on. If you have boobs, please check them.
Think boobs.”
~~~~~~~~~~~~~~~~~~
Prof John Newton
Chief Knowledge Officer, PHE
Cancer – A public health perspective
So many things to learn from what Kris was saying. Behind every statistic and data is a real person like Kris. This should be a reminder.
4 things we need to do:
- Prevention
- Diagnosing cancer early
- Make sure very patient gets the best treatment
- Care of people who are living with cancer, whatever the outcome
Struck by Cancer Research UK stats that 40% of cancers are preventable. There is a huge challenge but we as a population need to address it.
Good news is that we have the best treatment services and charities in the UK. We have some of the best intelligence systems in the world. The best Cancer Registry.
No doubt that cancer intelligence NCIN has played it’s part in improvements. More that we could do with the data to improve outcomes and prevent cancers.
How do we build NCIN in Public Health England to get even better outcomes?
Mission – “To protect and improve the nations health and to address inequalities working with national and local government, the NHS, industry, academia, the public and the voluntary and community sector”
Broken down into manageable chunks – outcome focused.
- Helping people to live longer and more healthy lives by reducing preventable deaths and the burden of ill health associated with smoking, obesity etc
- Reducing the burden of disease and disability in life by focusing on preventing and recovery.
- Protecting the country from infectious diseases and environmental hazards
- Supporting families
- Health in the workplace
- Promoting development of place based public health systems
- Developing our own capacity and capability to provide professional scientific and delivery expertise
PHE’s jewels in the crown:
- National Screening Programme
- National Cancer Registration Service
- National Cancer Intelligence Network.
PHE inherited some strong partnerships with many including:
National Cancer Peer Review and National Cancer Research Institute.
PHE have a significant local presence:
- 4 regions, 15 centres
- 8 cancer registration teams
- Central coordination and analytical team
- 8 knowledge and intelligence teams around the country
Track record of delivery is increasing….
- National Cancer Registration Service
- Completed the national migration
- Data going out trusts
- Published staging data
- Cancer analysis system implemented
- Prostate cancer data network
Our public health perspective:
NCIN
- Be clear on cancer campaign evaluations have been carried out for lung, blood in pee, breast cancer in over 70s, ovarian, oesophago-gastric, lung reminder and local skin cancer pilot.
- Analytical work by the central and knowledge and intelligence teams
- 16 data briefings, 23 in depth reports, 9 press releases
17 journal articles, profiles, toolkits, routes to diagnosis, workshops for clinicans…
- 16 data briefings, 23 in depth reports, 9 press releases
- New office for data release is established and now operational
- Reports analytics from the page impressions on our websites show an increase both nationally and internationally.
Collaborative work:
- Deprivation report with CRUK
- Routes from Diagnosis with Macmillan
- Less common cancers – Cancer 52
The patient portal:
- NCRS and NCIN
- Brians Trust
- Cancer Research UK
Summary/Future Look
- Cancer remains as a significant public health issue
- Many national cancer bodies inside PHE brings definite synergies, some of which we are now seeing, but there is much more to do… we want your help with it.
- Growing demands for our intelligence capacity
- NCIN will grow and flourish as a partnership and as part of PHE’s integrated cancer programme.
Increasing value to assets whilst data, partnerships and resources continue to flourish and grow. We need to work together to ensure that this data and these collaborations continue to demonstrate improvement for cancer outcomes.
~~~~~~~~~~~~~~~~~~
Sean Duffy
National Clinical Director for Cancer – NHS England
Progress on the delivery of optimal care for cancer patients in the new NHS
Optimal cancer care in the new NHS – an absolute commitment to deliver services for better outcomes.
The survival challenge
- Mortality improvements v survival gap
- Although we’ve made gains in the survival in the UK. Other countries have also had improvements. We need not to equal the other countries improvements but to ensure our improvements are greater.
- Eurocare 5 (2013 analysis of 2007 data)
- Stage at presentation and earlier diagnosis.
- We need a cultural and system shift to lead a stage shift.
- Primary care interface – % flows
- GP direct access to tests. Does it make a difference. On average access to test should make a difference for 6% cases. BUT hides 15-20% for cases such as stomach, ovarian, pancreas, renal, brain.
- Route to diagnoss, England 2006-2008
- All cancers emergency presentations 24%
Ownership of treatment decision
We should ask every MDT in every hospital to look at least once a year at the decisions it has made (treatments) and what it has meant for its patients (outcomes). By revisiting these decisions they may be able to see improvements or identify changes that need to be made.
National datasets for cancer should enable the work – chemo, radiotherapy and outcomes data
National audits need to be used more.
Transparency is essential
12 senate geographies for the cancer map. If they took a grip of their own survival curves then we could be in a better position.
Plea – Own your 1 year survival and work collaboratively together.
Selection bias
- Age and outcomes
- 34% of 80-84 and 43% of 85+ are diagnosed via emergency route compared to 25% of 70-79 year olds.
- Age and treatment
- Access to treatment of the older population is variable. There is an age bias that exists and the data sets demonstrate this. Not just for surgery but also chemo, radio and access to a cancer nurse specialist.
- Perhaps there could be a co-morbitity and late stage diagnosis but not completely responsible for decline in survival in older patients.
- Older patients get less chemotherapy delivery for colorectal patients.
Structure
- Key factors that influence greatest impact is access
- The question of volume and outcomes
- Community of care, not individual or isolated providers
- Redefine the model – ideal structure within given senate geographers based on IOG principles and evidence.
What is best and where?
Summary
- Gap in survival to tackle together.
- Effective plan for early diagnosis to ensure the front end of our health care system delivers what you need it to.
- Local MDT and senate geography focus on outcomes as a result of treatment decisions is vital to improve survival.
- There is an inherent age bias that if tackled could yield significant survival benefits.
- The evidence for volume linked to survival outcome cannot be ignored.
Q&A
Q (Kathy – London Cancer Alliance) – What has happened with the key recommendation in 1995 re early diagnosis? Ambition was to go much further than they did at the time. The data at that time wasn’t as robust as at the moment. We have to be driven by the evidence. Any change moving forward has to be with improvements.
A (Michael CR_UK) – Are you talking to your colleagues in Scotland Wales and N Ireland about how to tackle the problems as a UK wide problem?
We are an English organisation but we are doing as much as we can with the UK. Spoke last week with the Welsh Health Minister (who are producing a white paper which is very interesting). Certainly on research we are very keen to work across the UK. Every reason and possibility of working across the UK not just England.
Julia Vern NCIN public health lead – UK and Ireland Association of Cancer Registries – absolutely a priority for all of us.
Q (Bob – Former NHS professional and lay rep) – Where is recent data?
A – Pointing you to the right person for the data question.
Q (Ian – Patient) – Emphasis is always on the clinicians rather than the patients. If there was more of a focus on the patient not the clinicians then I think you would see more survival times. Supporting stop smoking, diet etc particularly those of the poorer socioeconomic groups.
A – I think you’re right. Workstreams should be looking at exercise and other actions as a joint initiative between NHS England and Public Health England.
Approach moves away from a health service that provides testament for someone who is ill, rather than helping patients help themselves before they become a patient… it needs collaboration with charities, education and health care systems.
Q (Ms Clifton – Clic Sergeant) – Early/late diagnosis. GP dismissal of patients. Is any research done on looking at the reasons for late diagnosis or sending for tests in primary care?
A – How long have we got? There is a lot of research and simple things that primary care have developed to be more proactive. Got plenty to base a plan and are working on it. Key for me is that this is about public and primary care behaviour. The new changes should enable us to have more conversations and changes in this area.
Kris – We ran a focus group with some GPs. Reduction of the younger patients and also looked at the flip side of empowering patients about what you expect from a GP visit. Makes a huge difference.
Q – (Sara Hyams CR_UK) – Pick up on the age issue. How do we get more on the agenda for early diagnosis of the younger patients? i.e. under 30. How can we also improve things at the other end of the scale too?
Q – CCG – when would staging data be available to CCG levels?
A – Staging data has already been published. By CCG I understand it’s going to be June. NCIN is publishing it later this month.
Q – Health intelligence officer – I’ve got a 23 year old daughter. All this activity around data and intelligence isn’t worth anything unless it is used for the benefit of the patients.
~~~~~~~~~~~~~~~~~~
Plenary 1 – Outcomes for young people with cancer: matching commissioning guidance with the evidence
Martin McCabe
Chair of NCIN Young Patient Oncologist
NICE guidance on improving outcomes for young people and children with cancer. (“CYP” children & young people)
- Care co-ordinated as close to home as possible
- Networks should meet the needs of CYP with cancer
- MDT should provide cancer acre
- Each CYP with cancer should have a key worker
- Care appropriate to CYPs age and type of cancer
- CYP with cancer should be offered the chance to take part in research trials
- Treatment should be based on agreed protocols
- Sufficient specialist staff
- A register of all cancers in people aged 15-24
National Registry of Childhood Tumours
Established in England, Soctland and Wales in 1962
Childhood cancer isn’t well fit with ICCD coding so they have their own code. Birch coding.
TYA cancer
Teenage and Adult with Cancer TYAC founded in 2004.
In children cancer is always rare. Rare because it’s found in a child or because it is rare anyway.
Looking at survival AND important is quality of survival for children and young people.
Treated at a Principle Treatment Centre… but what happens when they’re referred out of the PTC?
One of the main advancements in childhood cancers is the enrollment of children into clinical trials. New paper from NCRI to be published very shortly which demonstrates this.
~~~~~~~~~~~~~~~~~~
Kathy Pritchard-Jones
UCL London Cancer
Paediatric clinical outcomes research – UK policy and the role of the European Network of Cancer Research in Children and Adolescents – early diagnosis
Talking about the European agenda for paediatric cancer clinical outcomes research.
ENCCA European network for cancer research in children and adolescents 2011-15
SIOP European standard of care for children with cancer
ExPO-r-NET European Expert Paed Oncology Research Network for Diagnostics and Treatment
Outcomes research
- Outcomes seeks to provide evidence bout which intervention work best
- Study of the end results of health services to take account opatients experience and costs to society
- Provide scientific evidence
NHS Outcomes of framework
- What can we really measure that is important to patients?
ENCCA – in 4th year of operation
- Building a strategy to enable biology driven clinical and pre-clinical research. Tissue sampling, biobanking and sharing tissue across boundaries, training for clinicians, researchers and scientist. Long term sustainability of encca is bringing together national paed and cross cutting research groups to take it forward.
Why has overall mortality for children with neuroblastoma in the UK worsened? Is it because there’s no trial currently open?
Infants with cancer have the highest rate of early mortality. Can we improve their model of care?
Equal access across Europe. Appointed by DG-SANCO to pilot how cross-border research can be done correctly?
Collaboration, defining entities, regulatory, embedding teaching and research.
~~~~~~~~~~~~~~~~~~
Tony Moran
Public Health England
Survival trends for young patients in the UK – the good and the bad diagnosis
Background
Lower survival in UK than several other countries
Rate of improvement slower in TYA than other age groups?
[Once the presentation is available, I’ll upload it here]
~~~~~~~~~~~~~~~~~~
Kathryn O’Hara
The Christie NHS Foundation Trust
Referral to and from specialist Centres- how widespread is the practice?
Normal for 0-14 year olds to be under the principle treatment centres classified by extent of shared care. It’s not consistent in all areas.
~~~~~~~~~~~~~~~~~~
Plenary 2 – Living with and beyond cancer
Heather Monteverde
GM of Northern Ireland with Macmillan Cancer
Considering living with and beyond cancer is a newly adopted consideration… relatively. So many changes within cancer with chemo, radiotherapy, surgery etc.
Consequences of treatment or late affects have a huge impact on the quality of life of people living with and beyond a cancer diagnosis. This also needs to be addressed. The physical as well as the emotional and psychosocial issues.
~~~~~~~~~~~~~~~~~~
Raoul Reulen
Uni of Birmingham
Teenage and Young Adult Cancer Survival study
Approx 225,000 5-yr survivors
Population based cohort
Diagnosed 1971-2006
Age 15-39
Covers England and Wales
Study link
~~~~~~~~~~~~~~~~~~
Matthew Francis
Public Health England, Knowledge and Intelligence Team, West Midlands
Method of identifying stage IV cancer
Presentation – please refer for charts and graphs.
Matthew spoke about the differences in staging sarcoma compared to other cancers. The usual methods of staging include tumour size, nodal involvement and if there are any distant metastases identified.
With reference to sarcoma patients only 2% of those diagnosed with stage IV actually comply with these staging rules. This makes it increasingly difficult to make comparisons and potentially contribute to a less favourable outcome.
In addition the rarity of sarcoma:
450 bone sarcomas new diagnosis
2,800 soft tissue sarcoma new diagnosis
less than 1% of malignancy
occur in different anatomical locations.
Detailed staging data is not available for patients with sarcoma.
Metastases site recording in HES can be the only identifier but this information isn’t always recorded.
4,602 new cases of bone sarcoma
20% of had metastases at diagnosis
27,913 soft tissue sarcoma between 2000-2010
3,602 13% had metastases
Soft tissue sarcoma – some sites have space for growth i.e. abdominal or breast where the tumours have space to grow and therefore not diagnosed as quickly i.e. may be identified at diagnosis with metastases.
Conclusions
Staging data for sarcoma is incomplete.
Those with metastases have significantly poorer outcomes.
The methodology used to identify stage IV sarcoma patients could be applied to other cancer data sites and assist the National Cancer Registration Service.
~~~~~~~~~~~~~~~~~~
Chris Brown
National Cancer Registry Ireland
Using routine prescribing data to identify comorbidities in ovarian cancer patients
Please refer to the slides and data of the presentation.
~~~~~~~~~~~~~~~~~~
Plenary 2 – “Show me the data!” – information and intelligence for your ovarian cancer service
Chair: Annwen Jones
Target Ovarian Cancer
Ovarian cancer outcomes could be improved. NCIN has provided hard evidence that outcomes can improve and also provided data and insights to shape policy and practice.
7,000 cases diagnosed each year
3/4 of cases aged 55 years and over
4th most common cause of death from cancer in women
4,300 women die each year
Late diagnosis is a major issue
Before 2007 (i.e. before NCIN) we had very little and incomplete data that was also unreliable.
32% of women diagnosed with ovarian cancer via admission to A&E v 24% of all cancers
15% of women die within two months of diagnosis.
Pathfinder Study – Target Ovarian Cancer – 2009, 2012, 2015… ongoing study.
Looks at patient delay, GP delay and system delay.
[Key findings published to date click here]
International benchmarking partnership (ICBP):
1 yr survival for ovarian cancer in England lags behind comparable countries
5 year survival difference results from 1 year difference. In England we do quite well at this point.
Data shows that there are wide regional differences in survival.
What is the underlying cause of variation and what more can we do to improve survival for all women with ovarian cancer? What does the data intelligence that we currently have tell us? What further data do we need?
Put patients at the heart… policymakers, patient organisations, commissioners and clinicians around patients. The patient must be central.
The value of data to patient organisations:
Policy – impossible to influence policy without robust data.
Charity – we have to make sure that we’re spending the donations wisely. Data helps make decisions and priorities as a charity.
Patient choice – patients with a voice. Personal note – it was wonderful to see the faces of patients on Annwen’s slide particularly that of my gorgeous smiling friend, Tish, who I miss so very much. Tish was such a wonderful patient advocate for Target and others diagnosed with ovarian cancer.
~~~~~~~~~~~~~~~~~~
Dr Andy Nordin
Chair NCIN Gynaecological Cancer site specific clinical reference group
Ovarian caner in the UK: the emerging picture
ICBP – opportunity to compare outcomes with other high quality data countries such as Australia, Cancer, Denmark, Norway, Sweden 1996-2007
Gynae cancer hub with NCIN run through of projects carried out.
Results are improving in younger women but data identified that it hasn’t improved in the older patients. NCIN were then able to look at this area too.
Routes to Diagnosis in November 2010 we all know was that a great many people present as emergency presentation… ovarian is one that indicates this highly.
Short term ovarian case mortality:
- why the elderly
- late presentation
- reluctance for referral
- performance status
- patient preference
- access to specialist surgery
- access to chemo
- national variation
There needs to be more specialisation at a surgical level. To look at the number of consultants by caseload and acknowledge that they should be doing more than 15 cases per year. This surgery should NOT be undertaken by general surgeons but by specialist surgeons in specialist centres.
More use should be made of the cancer e-atlas
~~~~~~~~~~~~~~~~~~
Jason Poole
Associate Director, Public Health England
Short term ovarian cancer mortality in and across England
ICBP
Early results 2006-2009:
5288 women 31% died in the first year
2,592 died in first 2 months
3 contributory factors:
emergency presentation
advanced age
non-specific tumour morphology
case-mix analyses
- women 2008-2010 resident in England, ages 15-99
- data from national cancer data repository
- HES inpatent and outpaitient
- Ovarian cancer including fallopian tube and primary peritoneal cancers
- Excl borderline tumours, sarcoma, germ cell tumours
- 15,000 women in analysis
Patient outcome – excess mortality ie over and above ‘normal’ population mortality
3 periods of analysis – diagnosis to 1m, 1mto 6m; 6-12m
case mix factors
- age groups
- deprivation quintile
- comorbidity
- route to diagnosis
- stage
- morphology
- treatment
- basis of diagnosis
~~~~~~~~~~~~~~~~~~
Dr Rob Gornall
Clinical Director Cancer Services
The challenge of improving cancer services by commissioning pathways – the increasing value of data
Rob’s presentation reiterated a great many of the points earlier regarding early diagnosis, variation in primary and secondary care services, complex commissioning pathways, patient behaviour and perception of risk.
Please refer to the presentation for more data on the above but please note there are graphic photographs.
~~~~~~~~~~~~~~~~~~
Louise Bayne
CEO Ovacome
Robust data – the value to patients and patient organisations of the NCIN
Why is the NCIN data required and quality of it so important?:
- demographically representative
- statistically significant sample size
- non biased enquiry motive
- highly skilled practitioners
- published in full
Without NCIN data, charities need to look inwards for data sources and information. That has intrinsic problems about it. Attract a sub-set of the cancer community who are not representative. Might be questionable motives as to why a charity has come up with a news story or report.
Why does this matter?
Data is used for:
- NICE decisions on access of treatments.
- shaping research proposals
- commissioning
- advocacy programs
- patient information
- individual treatment choice
Without excellent data patient organisation activities risk being characterised as:
- opinion drive
- biased
- questionable motives
Leading to:
- wasted resources
- lobby fatigue
- harm to misrepresented clinical sectors
- poorer outcomes for community
Making the data count
- Quality profiles – annual report using NCIN/DH data to provide a local picture of service/standards
- Available on the Ovacome website
- Parliamentary outreach day with Ovacome members lobbying their MPs
- Circumvents clinical gagging clauses
- Puts clinicians in the driving seat – we don’t say what’s to happen – clinical empowered to suggest improvements
- Last year resulted in Secretary of State intervention, improvements to the data collection, the recruitment of clinical staff and improvements in clinical service (in one centre the development of a GP helpline)
The drive to improve diagnosis:
- the majority of women have advanced stage disease at diagnosis
- received wisdom – ovarian cancer is a silent killler – only symptomatic at advanced stage
But the studies said differently….
Using data for improving diagnosis:
BEAT campaign Bloating Eating Abdominal Talking.
Survivors teaching students
Commissioning – why NCIN is now essential
Commissioning challenges us to consider business as usual or optimal practice
To drive improvement trustworthy data is essential
However gaps in data remain a challenge