The second day of the conference began with me being fairly grumpy! The queue to get into the dining room for breakfast was stretching out to reception! After 20 minutes of waiting, I gave up. I only wanted a croissant and some fruit but it wasn’t to be as I was keen not to miss any of the conference… but no breakfast = grumpy Anna! Hilton Hotels get your act together!
~~~~~~~~~~~~~~~~~~
Plenary 3 – Global cancer surveillance: opportunities and challenges
Professor Julia Verne
Director of Knowledge and Intelligence Team SW, Public Health England
Plenary session in the memory of Brian Cottier (1951-2009)
1 in 3 will get cancer
1 in 4 will die from cancer
~~~~~~~~~~~~~~~~~~
Freddie Bray
IARC – International Agency for Research on Cancer
“World wide cancer burden”
Global cancer surveillance opportunities and challenges
Socioeconomic changes and how that impacts cancer incidence and survival.
14.1 new cases in 2012
8.2m deaths
32.5m living with a cancer diagnosis
9 cancers for majority of cancers 2/3rds of burden.
Globocan 2012 provides many graphs and examples.
The changing world – transitions
Major increases in the population coupled with increasing longevity has linked to epidemologic translations Including cancer, moving from infection related cancers toward a western lifestyle.
1 in 3 NCDs are cancers.
A great deal of information and graphs showing changes in some countries for increases in cancer and also decreases eg Japan have an increase in young people with cervical cancer. India have a reduction as marriage age is getting higher. Russia and Belarus have no screening and it has rapidly increased for cervical cancers.
Why registries are so important so we can track what is happening and measure it accordingly.
NCD agenda, of surveillance activities
Training and collaboration with cancer registries around the world. Try to ensure registries are in place to help with cancer control and also for reporting worldwide.
3 way split between high quality data, national and regional data and frequency data but 62 countries with NO data at all.
Current situation
Recognition of increasing global cancer burden.
Despite a long history of cancer registration LMIC have not developed PBCR
Link in with political agenda and tackling of NCDs
UN high level summit talks about cancer registries.
Global monitoring framework
IARC Technical Publication No 42 “Planning and developing population based cancer registration…”
Global Initiative for Cancer Registry objectives
IARC Regional Hubs for Cancer Registration in LMIC
Good data collection and methods of using and sharing data effectively.
~~~~~~~~~~~~~~~~~~
Dr Milena Sant
Instituto Tumori, Italy
EUROCARE 5 – survival of cancer patients in Europe
21 countries with a national registry inc 7 countries from eastern Europe.
50% of European populations including over 10m cancer cases.
Next steps for Eurocare
Reduce inequalities,
Treatment is not only solution for control
primary prevention, early diagnosis, accurate diagnosis – are all factors
~~~~~~~~~~~~~~~~~~
Sara Hiom
Cancer Research UK
The International Cancer Benchmarking Partnership’s Impact on Policy and Practice
What is the ICBP? – unique collaboration in terms of countries, international collaboration involving policy, research, cancer registry and clinical professionals at a global view.
13 jurisdictions in 6 countries
including Scotland for module 5
What are they looking at?
- breast, lung, colorectal and ovarian
5 modules
- Epidemiological benchmarking study
- Public awareness, attitudes and beliefs
- The role of primary care and healthcare systems
- Variation in patient,diagnostic and treatment time intervals and routes to diagnosis
- Data comparability and early deaths
Focus increasingly on the first year post diagnosis. Why are we not getting more patients beyond the first year survival which we can also see affects the 5 year survival statistics.
Module 1 – survival and stage table.
It’s not only early diagnosis that came out from this module and data comparison. It was also access to services and quality of treatment.
Module 2 – awareness and beliefs
Looked at differences in population. In the UK were our people less aware of the signs and symptoms?
Findings: ABC measure was born and has been used for surveying populations.
Generally speaking similar levels of awareness across all ICBP countries.
Generally low awareness across all countries of the increase factor of age.
UK – stood out the reluctance to visit a GP and wasting the Dr’s time. Elements of embarrassment i coming forward in the UK.
Be Clear on Cancer campaign to try to change the belief of wasting GP’s time or embarrassment.
Module 3 – role of primary care
Were there fundamental differences in systems?
- Progress 2895 GPs responses to online survey and analysis complete in 11 jurisdictions.
Papers are about to be published.
Latest (unpublished) international data suggests that GPs in England:
- Are less likely to send a patient for tests
- Report having among the lowest access to specialist advice
- Tend to feel more strongly about protecting their patients from over investigation and preventing a secondary care overload.
We need to look at the cost structure to overcome this aspect.
Module 4 – patient, GP and specialist intervals
Still underway…
- Looking at via surveys patients, GP and specialist.
- Looking at length of time between first noticing symptoms and time to GP and referral.
- Collecting this information across the cancer pathway in 10 jurisdictions and comparing each of them.
- Anticipated impact is focus in on areas with longest interval.
Module 5 – data quality simulation
Variations in cancer registry practices affect the comparability of key data used in cancer survival analyses
Look in much more depth of the differences in registries.
Should have a key impact on the best practices and developing tools that look at different factors.
Module 5.2 – short term mortality and co-morbidity
Not started yet…
Building on the legacy of ICBP. Lots of questions have left unanswered but needs to continue and keep it up on the agenda. Perhaps political policy will assist keeping it on the agenda particularly as comparing with other countries.
~~~~~~~~~~~~~~~~~~
Reducing Health Inequalities
Chair: Dr Tony Moran
Director of Research and Intelligence (North West) at Public Health England
~~~~~~~~~~~~~~~~~~
Therese Lloyd
Prostate Cancer UK
Lifetime risk of diagnosed with and dying from prostate cancer in different ethnic groups
Process of finalising a publication but as yet unpublished.
What do we know?
- 1 in 8 men in the UK will be diagnosed with prostate cancer at some stage in their life.
We know there are ethnic differences but don’t know how they translate into incidence and mortality.
Data and analysis
Few date issues that meant we weren’t always able to tell the ethnicity for over 1/4 of the data fields.
Total numbers of deaths in the data did not match up the total number of deaths in the office of statistics.
Several analyses in each ethnic group were done.
Best estimate but also larger groups to get a true value.
Used DevCan – system US.
Major ethnic groups analysed – white, black and asian.
Mixed – were difficult to obtain clear results.
Lifetime risk is calculated as percentage and odds.
Although there is a bit of variability based on the methodology used. Consistent message that Asian men (1 in 13) are at a lower risk of being diagnosed of prostate cancer than white men (1 in 8).
Black men are at a much higher risk, although much more variability the research evidences that approximately 1 in 4.
Best estimate – White 1 in 24, Asian 1 in 44 and black 1 in 12 – dying from prostate cancer.
Looked at data from 2008-2010.
When you compare the diagnose number and deaths all groups indicate that 1/3 (across board) will die once diagnosed. Perhaps there is no difference between the aggressiveness of the disease no matter what colour skin.
Need to reach out to BME communities to be aware of symptoms.
More research is needed and collection of perfect ethnicity data is needed.
~~~~~~~~~~~~~~~~~~
Chin Kuo Chang
King’s College London
A cohort study of mental disorders, stage of cancer at diagnosis and subsequent survival
2011 cancers has seen the largest percentage of death in the UK accounting for 30% cause of death.
For serious mental illness it’s the 2nd or 3rd cause of death.
Big gap between the general population and people with serious mental illness (‘SMI’).
Only 1 team in WAustralia investigating this.
2 research questions (looking at data 2010-2013) CRIS
early symptoms ignored or not understood. Is the stage also affected when diagnosed.
Cancer linkage
- Cancer register to include incidence of mental disorders
- Trajectories of cancer treatments for ppl with SMI
- Prognosis of cancer patients with psychiatric comorbiditiy.
Extending CRIS system to Cambriddge, Imperial – UCL, Oxford and Camden & Islington.
~~~~~~~~~~~~~~~~~~
Mark Rutherford
Research Associate, University of Leicester
Understanding deprivation and inequalities using loss in execution of life use to a cancer diagnosis (using only UK data)
Please refer to presentation
~~~~~~~~~~~~~~~~~~
Preventing Emergency Presentations – the need for research
Chair: Stephen Duffy
Wolfson Institute
We know that emergency presentation is particularly common in some cancers such as lung and bowel. Associated with a poorer outcome and may be associated with initial treatment from wrong specialist.
Emergency Presentation is more common in older people.
We need better understanding who’s at risk and what can we do about it?
Targets for today from the interactive workshop:
What are the major knowledge gaps?
What cancer sites are most promising for intervention?
What interventions are ready for evaluation?
Not simply to replace Emergency presenting with routine presentation. We want to replace with someone presenting 6-12 months before with stage 1 or 2 cancer.
Who should take this forward?
Very much in our hands as to which teams should take these interventions forward? Research fellows? Charities?
~~~~~~~~~~~~~~~~~~
Less Common Cancers
Chair: Jane Lyons
Cancer52
Cancer52-NCIN-Report-10-June-2014-FINAL
~~~~~~~~~~~~~~~~~~
Lucy Elllis-Brookes
NCIN & PHE
Setting the scene for rare and less common cancers
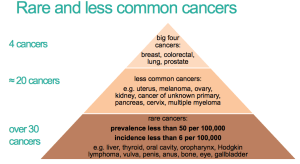
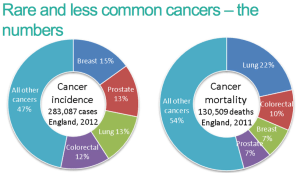
Big 4 – breast colorectal lung and prostate
Less common cancers e.g. uterous, melanoma, ovary, kidney, CUP, pancreas, cervix, multiple myeloma
Rare cancers…. even more !
What is NCIN doing?
Routes to diagnosis – increased look at cancer types and producing data from them 22 in 2010 and 57 in 2014.
Deprivation reports – 23 in 2008 and 37 in 2014
Site specific Clinical reference group work (recent examples)
- vulval cancer – trends and variations by age
- kidney cancer survival report
- penile cancer incidence by age
What do rare and less common cancers have in common?
- Each cancer site shows different results.
- Different analyses will be required
- Specialist advice (clinical and analytical) is crucial.
~~~~~~~~~~~~~~~~~~
Oksana Kirichek
University of Oxford
Menopausal hormone therapy and risk of central nervous system tumours: a nested case – control study
Aim of study:
- Is Hormone therapy (HT) associated with risk of brain and other CNS tumours
- To test whether the effect of HT varies type, duration or recency of HT preparation used.
- To assess the effect of HT exposure on the risks for all CNS tumours
GPRD General Practice Research Database
- Holds primary and secondary data. cross linked with other databases and person specific.
Definition of cases
Results
No significant difference in risk by tumour subtype
Conclusions
- UK GPRD cohort women who had been prescribed HT
- HT associated risks did not vary significantly cross the four main tumour subtypes examined
- Findings from the GPRD agree with those reported previously from other studies with prospectively collected information on HT use.
~~~~~~~~~~~~~~~~~~
Nicola Dennis
Knowledge and Intelligence Team (W Midlands)
Incidence, survival and treatment patterns for patients with head and neck sarcoma
1% of all malignancies in England are Soft tissue sarcoma
Narrowed down to head and neck the numbers are even smaller
With the very small numbers of incidence there are limited studies looking at incidence and survival rates.
Both Improving Outcome Guidance in 2004 and 2006 specifically had improvements for head and neck.
Because of the small numbers its hard to see if anything has changed.
4796 head and neck sarcomas in 1990-2010
MDT specialty – positive outcomes since the guidance was set out where we can see that there has been a significant increase in referral to the right MDT specialty.
Patient spread for surgical treatment. Data shows that there are number of trusts that might only have treated 1 patient in the entire 10 years of the study!
~~~~~~~~~~~~~~~~~~
Kwok Wong
University of Birmingham
Risk of Adverse Health and Social Outcomes up to 50 Years After Wilms’ Tumour: The British Childhood Cancer Survivor Study
I will post a link to the presentation once available.
~~~~~~~~~~~~~~~~~~
Plenary 4 – Delivering outcomes that matter – Panel debate with Q&A to the panel
Chair: Robert Peston, BBC’s Economics Editor
• Mr Sean Duffy, National Clinical Director for Cancer Services, NHS England
• Mr Ciaran Devane, Chief Executive, Macmillan Cancer Support
• Professor Peter Johnson, Chief Clinician, Cancer Research UK
• Dr Jem Rashbass, Director for Disease Registration, Public Health England
• Mr Andrew Wilson, Chief Executive, Rarer Cancer Forum

Ciaran Devane – Chief Exec – Macmillan
We need to move to a strategy when we think in a different way rather than the economics.
We are talking a great deal about the value of services and NHS etc rather than the value of and to the individual.
Changes in the NHS – are we spreading our resources too thinly?
Sean Duffy – National Clinical Director for Cancer NHS England
No doubt the point of contact for you within the health service should be the most important thing. We’ve not yet got it right. If we’re going to visit better outcomes then we need to tackle the first point of contact too.
We don’t wrap the system around the patients enough.
In terms of the data itself – it’s easy to look at national data and say were good at this or that. We can look at a local level. We need to create ownership of the data around the geographies to be sure their own data is better and is owned. Working collectively to gather for the greater good.
Rich national dataset that we can and must use but we haven’t yet made great inroads in it. Need to make more out of the data.
Finally, with such a rich set of data and the ability to intelligently obtain information from it. We need to get cleverer at using the data in order to year on year look at the services to ensure we can achieve the best.
Prof Peter Johnson, Chief Clinician, Cancer Research UK
Echo the good things said about NCIN and the work they do. No doubt research using the data has been saving lives for many years. We know more about how to reduce the risk of cancer and determine the best treatment and long term outcomes.
How are we going to improve further and get up and beyond the levels of other countries?
We know there are at least 10 different types of breast cancer. We know asbestos causes mesothelioma.
Key obstacles we need to address: Regulation – looking at EU regulations and ability to track patients through system and outcomes will be compromised if EU data systems come in. We must at all costs make sure work is not held down by regulations.
Changes in the health systems recently has given us problems. Relationship with the information centre CPRD and difficulties of joining different data has given us delays and loss of capabilities in the Registry. This has stopped us doing as much as we would have liked and can achieve.
Public perception of data and it’s management has been undoubtedly damaged by care.data. This was a fundamental problem and unsettling. We have to overcome this. There have been ZERO breaches in any confidentiality of the Cancer Registry.
25% to 50% alive 10 years from diagnosis of cancer. CRUK want to bring this to 75% in the next 10 years. We need data to understand this and move forward. Stratified medicine has to understand at a detailed molecular level. We will only be able to capitalise on that if we can get the data systems right and keep them functioning.
Data is a precious life saving resource. Do not take it for granted. Fight to maintain the system that we have.
Dr Jem Rashbass, Director for Disease Regulation PHE
Worth reflecting on how we got here and what this is about We have had earthquakes of public trust. This is YOUR clinical information that we collect and we are duty bound to look after it and my responsibility to make sure that I protect patient confidentiality.
As Peter has said the support we’ve had over the years to look after your data and you can request it’s removal from the Cancer Registry.
This is about delivering care to individuals. You’ll treat them on the basis of the stats but as we move to personal care it’ll be the molecular abnormalities that determine your outcome.
We need to maintain the public support for data collection and NCIN database that puts the potential for cancer care in this country further forward than anywhere else in the world. In the next 5 years we will have extraordinary ability to provide the most personalised cancer treatment.
Andrew Wilson, CE Rarer Cancer Forum
Current state of play for data. Clear that public feeling has been shaken. Rarer cancers are rare. Data on rarer cancers will be much more identifiable. Huge amount of exciting work going on using data for rarer cancer.
Use of data in rare cancers. Hidden cancers and less visible to the public.
Huge demand for this sort of data. Need to meet this and produce reports that are useful.
NCIN route for diagnosis project showed ongoing problems for cancer patients go far beyond those related to cancer.
We need to be much more open with the data that we hold. Ensure patient identifiable information is removed from data sets. Once this has been done the data that we have is published. Closed shop needs to go. Automate data flow around the system to ensure sticking to rules and make better use of data that we do at present.
We need to work collaboratively to come up with solutions where problems exist.
Q&A
Q – How can we ensure the diagnostic experience for young people is improved?
SD – we have a first point of contact system designed 60 years ago. We need to tackle it externally and internally. Simple things needed – proactive approach to primary care. Safety netting – young person with a set of symptoms its probably the last place they want to be… be proactive and should raise a flag for tests. We have created a mechanism whereby the referral is the only route – needs to be challenged. GP should be able to make a clinical decision on the basis of facts not ask the patient to wait!
JR – We need to recognise that a missed diagnosis is one that everyone inc GP regrets. However some cancers in a young person are difficult to detect. They are rare. Symptoms and signs of a brain tumour are subtle. No of patients that a GP sees with those every week, it’s difficult to identify. Where the value of the dataset comes not from surveillance but that we should learn from every case. How do we raise our game?
SD – there are risk assessment tools that allow patients to flag up symptoms.
You can start to identify in an active way any of the GP patients that maybe at higher risk using some of these tools and data set.
RP – GPs feel they don’t have the level of control and responsibility due to other constraints about referring and cost.
CD – The guidance at the moment is written to say send us these patients but often the ones that don’t fit that mould are overlooked because they don’t fit that picture.
Be Clear on Cancer – enables the patient population community to know what to ask for and what symptoms.
PJ – I think there is a massive amount of data that tells us a lot about patterns of referral. And the outcomes from this. Feeding the information back into the system is incredible important.
Q – As a researcher the amount of time it takes to get access to data approved throughout he current regulatory approval system. Is there a strategy to help researchers get access to the data and make use of them in a more timely way.
JR – Richard’s experience shared by others. We’ve tied ourselves in knots frightened about releasing data and protecting the confidentiality. We need to recognise what you want us to do. Inside PHE we are trying to deal with it and create the structures to manage the data release. The demand for the data is large. We have disadvantaged ourselves by separating the people who pull the data and those who analyse it.
I think we do need a clear process of maintaining that public confidence.
Complex area but we need to be better at giving data confidentially.
RP – What is your attitude to selling data?
JR – Govt data is not available. Not a resource from which to make money. The data that we collect on you is for the social good BUT need to protect patient identifiable.
Financial constraints on delivering personalised health care will not be cheap. We need to enter into the discussion with industry to pay a fair price and benefit.
Q – How big a threat to our ability to gather and use data would changes be that require consent to use the data each time? This would negate the value of a Cancer Registry.
A – It’s a risk and will undermine everything that we’re trying to do. We need our MPs to change this view and to ensure that this change does not take place.
Q – One of the ways that we can prove that consenting to use of data is to show the public how the data can be used for good and can be done.
CD – Hugely disappointed when cancer networks became unpopular. People didn’t believe in coordination. We need to make use of the strategic clinical networks. Make sure the patient voice is embedded in the senates, and clinical settings. We need to be more assertive and move together.
JR – Some basic processes. Transparency and openness. Audit – any patient can approach and ask who looked at my data. Every patient who wishes can have access via a patient portal like the brain hub. An absolute right of opt-out. No process that makes it difficult to do that. I think that is what is needed to protect the data set that we’ve got and we need the community to act and educate the wider audience.
Q – Despite significant Govt rhetoric influencing the NHS work we need to collect ht patient voice at and put it back into the system. How can we go about changing this?
SD – I believe in the patient voice entirely. Within NHS England the patient survey is the most successful at influencing. We need to make more use of it.
Q – NCIN was founded in 2008 with mission to provide the UK with the best intelligence in the world. What does the panel think the new mission for the NCIN should be to take us forward in th next 5 years.
JR – We need to move somewhere else. I want a low level objective to make the patient and the clinician at the centre of the data store. So you can ask where am I in the system? You can check you’re getting the best and ensure that no cancer is left out. Patients and the public at the centre for cancer.
RP – When you collect data that is at a granular level are you recording it?
JR – Yes we are. We need to know what receptor it has. If it responded to medication. etc etc. Absolutely linking it into all sorts of datasets to look at a much bigger picture and make it more personalised.
PJ – 4 years of outstanding progress and 1 year of challenge. I think it’s time to reaffirm the quality of the data and now we need to see it and put it in front of the people who generated it, people, public, patients, clinicians etc. Want to see equally superb access to it.
CD – based on outcomes not last year’s data.
Q. – When a patient comes into hospital with advanced cancer, the patient has rarely been recording if they’ve been attending primary care prior to emergency presentation?
Should we incentivise GPs by giving them QoFs? Perhaps to embed good practice for a period of time.
PD – Both London integrated cancer centres have been involved in looking at attendance of A&E and that will give us some answers about the gaps. I do think there is something about incentivising a better pathway of care. We need to use everything in our power to make the system work.