Notes from my attending the NCIN conference – Liberating Information, Improving Outcomes – 15,16 & 17 June 2011
[Update – 23/08/11 – www.ncin.org.uk/news_and_events/conferences/2011.aspx for all the slides and presentations from the conference.]
NCIN (National Cancer Intelligence Network) – great source of data information relating to cancer. However worth noting that although they’re leading the way in collating cancer statistics (worldwide) we still have some way to go in order to feel we have complete information. For example, they can collect details about radiotherapy but not chemotherapy (a project to pull this info from relevant sources is underway).
Number of tools at http://www.ncin.org.uk/cancer_information_tools/eatlas.aspx (not all available to the public as need reporting tools however plenty to pull together!)
Very interesting Data Briefings reports including one about screen-detected breast cancer (Apr 2011) and one that means more to me regarding soft tissue sarcomas… but there’s plenty there.
There’s also a very useful booklet that NCIN have prepared (and you can ask to be sent to you via enquiries@nicn.org.uk) called ‘What cancer statistics are available, and where can I find them?’ or I’ve found the download at www.ncin.org.uk/view.aspx?rid=664
I saw a number of presentations by members of the South West Public Health Observatory and also chatted to them at their stand. Some very valuable and useful information in their ‘hubs’, worth promoting and also spending time rummaging for info, resources, profiles, data etc etc The Skin Cancer Hub, there are links to all sorts of other info and hubs, and early diagnosis info, stats etc at www.swpho.nhs.uk/ Their End of Life Care info is also really in depth.
~~~~~~~~~~~~~~~~
DAY 1
Plenary session: Improving outcomes for cancer
Chair: David Ardron, Chair, NCRI Consumer Liasion Group
Paul Burstow MP – Minister of State for Care Services
(personally I have a lot of time for Paul – he’s a straight-talker, knows his stuff and quite obviously cares about improving things too!)
UK are still behind the rest of Europe for cancer services and outcomes… however this has narrowed for breast cancer and it was felt that this was due, in part, to more awareness and campaigning by the BC community – so well done all!
Equity & Excellence Paper quite clearly showed in 2010 the need for an information revolution within the NHS and it was good to know we are some way there!
The paper also looked at:
- Linking information between health organisations, primary and secondary care, hospital episodes etc etc
- Recognising information to deliver improved quality of care
- Guaranteeing access to your own information
- Supporting patient, carer AND choice
We know that presenting cases via A&E ie worst diagnostics at primary care lead statistically to a poorer survival rate. Therefore one of the main areas we can change this is in education of the general public to be ‘body aware’ AND to present early to GPs but also to ensure that the primary care ie GPs are also aware of symptoms, tests, diagnostic tools etc.
There is also a piece about ’empowering’ patients to push forward if they know something isn’t right to ensure that if the GP sends them away with a ‘don’t worry’ that they go back or seek a 2nd opinion!
Data collection is now captured for metastatic disease in England. This is an area that previously we didn’t know about and one that will aid enormously with understanding the long term ‘survival’ requirements for our growing population and also how to manage the metastisised disease. (Again something that England lead on!)
Paul also spoke about evidence of equalities within cancer and producing data for cancer equalities that look at age, demographic, socio-economic, ethnic etc groups and the ability to slice and dice the data so that specific areas of inequality can be addressed head on.
~~~~~~~~~~~~~~~~
Mike Birtwistle – MD MHP Health Twitter @mbirty
He presented the ‘Brian Cottier Invitatio Lecture‘ I won’t summarise as the slides are in themselves v useful but if you need any more insight, give me a yell.
He also spoke about accounting for quality to the local community – http://www.kingsfund.org.uk/publications/quality_accounts.html
And also mentioned Joanne Rule and her patient review on patient experience. I found this and thought you may find this ‘interview‘ useful.
~~~~~~~~~~~~~~~~
Harpal Kumar, CEO, Cancer Research UK
Harpal spoke about where we need to be with regard to saving lives. He said that the Reform bill refers to improving our statistics to save a further 5,000 lives from cancer. However as he points out, if we were to do that, we would still only be at an ‘average’ within Europe which wasn’t good enough.. so in fact we need to save 10,000 lives to match the best. He also said that of course those countries will also be trying to save more lives so we should aim much much higher than that also!
He spoke about spearheading stratified medicine in the NHS and I’ve found a link on the Cancer Research UK site which explains a little more about what is meant by this. The diagram is key to understanding how the data and information for each and every patient can go toward ensuring we’re improving and the flow of the study and patient details.
Currently it will cover 9,000 people within the 6 main tumour types however it is intended that by 2015 all cancer patients and all tumour types will be included.
~~~~~~~~~~~~~~~~
Dr David Forman, Head of Cancer Information Section, IARC
Global cancer statistics – http://globocan.iarc.fr/
David spoke about his role and what he and IARC do with regard to cancer information and global comparisons.
In the UK:
310,000 new cases each year – 156,000 cancer related deaths each year
Globally:
12.7m new cases each year – 7.6m cancer related deaths each year
Prediction for 2030 (based on growth and ageing of population)
In the UK:
400,000 new cases each year (29% increase) – 210,000 cancer related deaths each year (26% increase)
Globally:
21.4m new cases each year (69% increase) – 13.1m cancer related deaths each year (72% increase)
Within the developing world the increase is 81% whereas in the developed world it is 34%
2011 UN summit on non-communicable diseases – he spoke about cancer being focussed on at this summit. WHO Global status report
He also spoke about their data collection tool CanReg5 being used in multiple languages to obtain the information needed.
~~~~~~~~~~~~~~~~
Workshop 1 – Less Common Cancers
This workshop was hosted by Simon Davies of Cancer52. Cancer52 is so named because of UK cancer statistics… 52% of UK cancer deaths are from the less common cancers – bet you didn’t know that? Do also take a minute to look at Cancer52’s website and promote and support them whenever you can… they do a fantastic job with very very little funding. Simon also heads up the Teenage Cancer Trust.
As those of you know I was diagnosed with a rare cancer, Cystosarcoma Phyllodes, in 2009 of which there is very little information, clinical or medical data or indeed a path upon which to travel or guidance on surgery or treatment. Rare cancer is therefore of particular personal interest…
So to the workshop…
Simon spoke about the incidence of rare cancers decreasing however the mortality due to rare cancers is increasing. Surely this should be investigated? Why would mortality increase and incidence decrease unless we’re simply not investing enough in research and trials?
This statistic is also somewhat surprising as Cancer of an Unknown Primary (“CUP”) was also not being recorded until 2008. This is a huge improvement in the collation of data to know that CUP is now being recorded (and ranks 2nd on the list of less common cancers) as this will once again be able to highlight the importance of investigation and research into CUP cases to perhaps better identify how/what/when/where the cancer can be classified.
I was also a little surprised to hear that only 20% of research funding and clinical trials is invested in less common cancers. This seems particularly low given that the incidence and mortality rates aren’t reflected in this investment. However perhaps this is due to each and every one of the rare/less common cancer organisations and individuals working for much smaller numbers and perhaps being a smaller voice in the shout for funds/trials! This is really where an organisation such as Cancer52 can help. Joining all the smaller charities and organisations together in order to have a voice has got to be the way forward and one that I thoroughly endorse.
~~~~~~~~~~~~~~~~
Chris Carrigan of NCIN
Chris spoke about their Cancer e-Atlas This tool allows you to select different areas in England, the cancer type, incidence, mortality, survival and then to compare with other areas in England. This tool and the data therein are being used to assess local prevalence of cancers and could again be used for commissioning in the locality. In addition the data for mortality will also be used and compared as this may give indicators about specific areas needing further help/assistance/specialist cancer hospitals or perhaps better emergency service responses!
This tool should be used in conjuction with the Cancer Commissioning Toolkit which is accessible by many listed medical groups including GPs and other health professionals.
Chris also spoke about a GP Practice profile. This tool is aimed at both GP practices themselves but also the PCT/Cancer Network GP Practice Profile/Audit Leads to be able to drill down to a practice level and see what that practice is doing with regards to cancer patients. They will also be able to compare themselves to other practices within their area and it is hoped will be able to identify areas of weakness that perhaps can be addressed by training or other initiatives. An example GP report
Once again the subject of good data arose… we need to get all health professionals entering data about patients into their systems accurately and completely. As well all know from our own lives, sometimes its easier to keep things in your head or scribble a note down however if the information is recorded accurately this will then allow organisations like NCIN, Thames Registry and others to collect, collate and analyse that data and to utilise the results in making a better health service for all.
However really exciting is that they’re collectively working toward getting all the information together into one Cancer Registry (ENCORE) with a target date of complete data by 2012/2013. Not a small task but one that is acknowledged by all as being crucial to tackling cancer head on.
~~~~~~~~~~~~~~~~
Ovarian Cancer Surgery by Specialists in Specialists Centres
John Butler, Dept of Health and Carolynn Gildea, Trent Cancer Registry
Ovarian Cancer is another that is grouped as a less common cancer however the incidence -v- mortality rate are shockingly bad. Last year 6,000 new cases were diagnosed with 4,000 deaths! Often these deaths are due to late diagnosis and emergency admissions rather than via GP practices. I know from friends diagnosed with this rare cancer that they had to return to their GPs on a number of occasions and ended up being diagnosed after presenting to Accident & Emergency. If you don’t know what the symptoms are, please take a minute to look at Target Ovarian or Ovacome.
John and Carolynn’s presentation was on the use of specialist surgeons for Ovarian cancer and more particularly whether the recommendation of “Surgery for ovarian cancer should be carried out by specialised gynaecological oncologists at cancer centres” in ‘Improving Outcomes in Gynaecological Cancers (DH, 1999) does lead to better outcomes for ovarian cancer patients.
Using data collected from 2000-2007 they presented a great deal of statistical information to support this finding however with one caveat… how is a ‘specialist gynaecological oncologist’ defined! It appears that some oncology surgeons are ‘adopting’ this title as they have performed this surgery regularly and have in turn being specialist in their medical facility. What their evidence showed however was that the there was an optimum amount of cases that a specialist surgeon does in order for the outcomes to improve and therefore a ‘specialist gynae oncologist’ who only performs this surgery a few times in his medical facility may not in fact be the best person to be seen whereas a specialist with many cases in a specialist hospital would be preferable as they not only do the work regularly but also have additional knowledge and back up in their medical facilities. John and Carolynn did however acknowledge that further investigation and perhaps classification should be undertaken so that anyone seeking information or guidance with regard to where to have surgery will have all the facts to hand.
But to summarise – they felt that a patient receiving surgery from a specialist gynaecological oncologist & in a specialist medical facility had a better outcome (and this was reflected in the statistics).
~~~~~~~~~~~~~~~~
Defining Soft Tissue Sarcomas
Matthew Francis, West Midlands Cancer Intelligence Unit
I was really buoyed to hear that West Midland’s Cancer Intelligence Unit is the lead registry for sarcoma in the UK.
Matthew’s presentation was particularly about the epidemiology of soft tissue sarcomas. Looking at how they are classified and also the process involved in their classification and use. He spoke about the importance of educating those parties responsible for data entry to ensure that when a sarcoma is identified they are classified correctly, leading to better reporting, analysis and it’s hoped outcomes. Matthew spoke of the importance of morphology codes to be used in addition as there are so many soft tissue sarcomas that could fall within one ICD-10 category. He also mentioned that most sarcomas are entered as C49 codes.
Particular interest to me as the classification codes that I was told Cystosarcoma Phyllodes had were M9020/0 D24 – Benign; M9020/1 D48-6 – NOS; M9020/3 C50- Malignant. So there’ll be no mention of either ICD-10 nor C49 in those codings! I will be following this up with Matthew and obtaining a list of soft tissue sarcoma classifications in the UK.
One thing that I learnt from Matthew’s presentation was simply that there were so very many different types of sarcoma but also that the importance of accurate data input and classification was crucial if we are going to see improvements in this growing area of rare cancers.
~~~~~~~~~~~~~~~~
Specialisation of Treatment of Bone Sarcomas in England (2000-2008)
Sally Vernon – West Midlands Cancer Intelligence Unit
Sally was asked to speak about the guidelines in the Improving Outcomes Guidance that recommend sarcoma care be managed in specialised units.
In short, what Sally found from her research and investigations is that there isn’t enough, up to date or accurate data in order to analyse if a patient diagnosed with a bone sarcoma has a better outcome by being treated in a specialist centre. From the figures she was able to ascertain she believes that approximately 40% have no record of being treated in a specialist centre however believes that the figures are inaccurately recorded and therefore analysed. Sally said that a great deal of patients aren’t diagnosed correctly or indeed treated as they often will be from a more elderly population or perhaps have a ‘fall’ and a break is recorded rather than a bone sarcoma identified at an early stage.
The learning therefore from Sally’s presentation was that, once again, we need better, more timely and complete recording in order to assess the value of specialist centres for bone sarcomas.
Predictors of Use of Orthotopic Bladder Reconstruction after Radical Cystectomy for Bladder Cancer: Data from a pilot study of 2414 cases 2004-2010
Luke Hounsome, South West Public Health Observatory
I won’t go into the presentation in length… but suffice it to say that we need better, more accurate, timely and correct data in order to analyse this well!
One final point that was mentioned during this session:
NCIN for patients and the public – are currently recruiting for new consumer members for their Site Specific Clinical Reference Groups – could you help?
~~~~~~~~~~~~~~~~
DAY 2
Plenary Session: Innovation
Chair – Dr David Brewster, Director, Scottish Cancer Registry
A new single registration system for England
Dr Jem Rashbass, National Director for Registry Modernisation
Jem spoke about work which is underway to pull together all cancer statistics into one system in a quick, accurate and efficient way. He also spoke of the importance of this information and that information is key to moving forward and finding answers.
“We need near real-time, cost effective and comprehensive data”
- consistent data (including staging)
- central data-sets
- Real-time QA
- Expandable
- Improved data access and timely feedback
- Seamless links to cancer screening
He spoke further about ENCORE the central registration system and that this will provide timely feedback to clinical teams along the patients entire pathway. AND that this data in and information out must be two-way.
Information collection data retrieval
He also spoke about the many ways that this information will be retrievable and the importance of being able to pull out reports in many different ways and at different reporting levels… I was very pleased to hear that these are all being considered and consulted upon in the build/implementation phase.
~~~~~~~~~~~~~~~~
Ciarán Devane, Chief Executive, Macmillan Cancer Support
Ciarán spoke about the patient experience. Something that I believe in so much is patient choice and patient experience, so my ears were pinned back!
[Although I did have to have my own little giggle when the Andrew Lansley quote was wheeled out ‘No decision about me, without me’… which was said at a time when the new health reform was announced… without proper patient consultation!!]
I’m going to bullet point some of the highlights from Ciarán’s talk:
- National Cancer Patient Experience Survey 2010 identified that the patient experience for those diagnosed with rare cancers were the worst.
- Evidence that if a patient has a Cancer Nurse Specialist assigned to them, their overall patient experience was better.
- There are 2m people living with and beyond cancer in 2010. On an assumption that this compounds at 3% per annum, this will mean that by 2030 we will have over 4m people living with and beyond cancer in the UK. Therefore the urgency of getting effective data and in a scalable way accurate and timely way, will assist patients and health professionals to manage to growing cancer population.
- We need to work with the workforce in the system to ensure good training; intervention and support.
- Personalisation for each person diagnosed and those affected by someone’s diagnosis. We also need to be better at self-management and provide the tools and services to do so. A great deal can be achieved by empowering patients and their carers.
- Choice. Every cancer patient has a choice in the UK about where they are to be treated however often the information isn’t available or the patient doesn’t feel comfortable asking for statistics, reports and information. Ciarán would like to see this information available and accessible so that patients are able to make the right choice for them at that time… in an informed and empowered way.
- Data collection – this should be a collaborative function between the Registry, clinicians, health professionals, patients and carers.
~~~~~~~~~~~~~~~~
John Baron MP, Chair of the All Party Parliamentary Group on Cancer
John wanted to speak about the three main aspects of the Reform Strategy:
1. Outcomes with the focus on improved outcomes.
2. Patient Empowerment
3. GP commissioning
1. Outcomes
He spoke about the first year survival rates being an area to focus upon. For instance statistically if we can improve the first year survival rates then the overall survival improvement will follow. We know that there is a direct correlation between late diagnosis and lower first year survival rates. We also know that 25% of diagnoses are made via A&E. We know that this is in part due to people being unaware of symptoms or perhaps putting off a visit to the GP however we also know that, particularly in the young, GPs are quick to assume that a person is too young to have cancer and turn them away, only to repeat a visit or the need for A&E.
John, once again highlighted the importance of early detection, symptom awareness, knowing your own body and of course, GP and health professional training.
2. Patient Empowerment
The Reform Strategy speaks about the a patient having choices. John went on to speak about the importance of those choices being jointly made with health professionals based on information and choice available. But also he acknowledged that many patients feel worried about asking for referral to specialist hospitals or second opinions and we (ALL) must ensure that patients are comfortable with asking. It is never a criticism of your current hospital but in fact a way that you can choose the best treatment/surgery/hospital for your requirements. This decision may not come down to medical factors but simply geography ie being nearer your family or friends for support and follow up appointments.
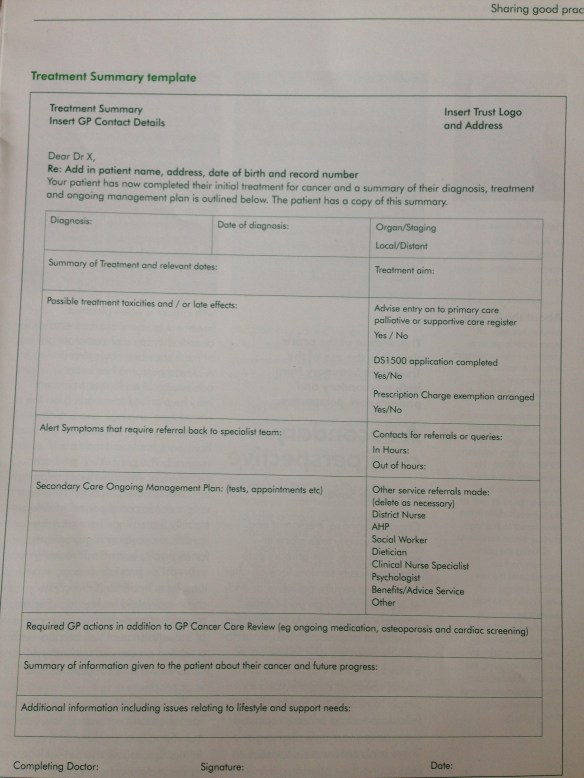
Patient Information Prescriptions should (and will) also be available for all cancers. At each part of a cancer pathway, from diagnosis to death (and may that be a very very very long time between!) that a patient, carer and health professionals are able to obtain information on a particular part of a pathway pertinent to that moment’s requirements. The National Cancer Action Team are working on this and have made great inroads into the project. There has been a slight glitch with the ongoing addition of documents and Stephen Parsons from NCAT explains a little more in a letter. However they are committed to making this happen… As a patient reviewer of the information documents, I am also a firm believer in the system. You can, from CancerInfo site see the pathways that are already live and download relevant information. Click on Pathways and then choose a pathway. You will then see a number of sections and by clicking on the blue + this will open up to show the documents available at that point in the pathway. For example Melanoma has 8 different sections each with varying number of documents available. You can view online or simply tick a checkbox of the information you wish to download and then save/print those documents you wish to view at the time. There are also triggers within the system that mean a document reaching 6 months of age is removed from the system until validated by the originator. NCAT are also working with charities and organisations to ensure we have combined information available to patients. Often we find that each charity has their own leaflet on a particular pathway and the information can be confusing to the patient.
Part of the project rollout is to ensure that at each point this information may be needed there is a printer and trained staff to talk through what the information means and provide a ‘pack’ to person in need of help and guidance. This is also carried out in holistic way so not only addressing the medical aspects but the emotional, psychological aspects of the patient.
3. GP Commissioning
Many people within the cancer field are concerned that the new GP commissioning structure will mean that specialist cancer services are not considered in many areas. However John was quick to say that these were being considered, tackled and planned out so that no matter where you are in the UK, you will have access to GP services through the new structure.
He also spoke about it being a collaborative method that was needed to ensure that the best services were available to all needing them.
John confirmed that Cancer Networks now had guaranteed funding for another year – something that was a concern that these networks, which being patient voice forward, might lose their funding.
Two questions that were asked by patient attendees were:
“Why aren’t patients represented on commissioning groups?”
“If a large part of missed early diagnosis falls with GPS, why are we going down GP commissioning for cancer services?”
Apparently these are both being addressed and patients being included however I would urge each of you to keep plugging away locally to ensure the patient voice is heard and included in commissioning at every level.
~~~~~~~~~~~~~~~~
Morning Workshop
Survivorship – a patient-led session (in partnership with NCRI Consumer Liaison Group)
Chaired by Ray Murphy, National Cancer Partnership
Ray ran through some the stats we’re getting to know so well. 2m people living with and beyond cancer now. 4m people living with and beyond cancer in 2030.
Cancer affects:
– physical, social, psychological… and so much more.
– patient, family, carers, colleagues… and so much more.
~~~~~~~~~~~~~~~~
Cancer Survivorship in the UK
Jacob Maddams – Thames Cancer Registry, Kings College London
Jacob examined data from 1990-2006 together with HES (Hospital Episode Statistics) from admitted patients in 2006 and this data was linked at a patient level.
I don’t think there was much more that Jacob added to the statistical evidence that has been provided previously and as above however it was so clear, once again, that we collectively, need to get smarter, faster and more accurate with our data inputting so that we can really analyse and use the data!
Increased risk of skeletal and cardiac events in prostate cancer patients
Luke Hounsome, South West Public Health Observatory
Luke’s presentation was looking at the data around prostate cancer patients and particularly the use of hormone therapies used with advanced or progressive types of prostate cancer. Although, sadly, once again it was evident that the data was incomplete as a number of the ‘watched patients’ were lost after a certain point leading a conclusion that Luke couldn’t specifically link a death to the treatment as it may have been inaccurately recorded for this evidence purpose. However that said, there was enough evidence to report that prostate cancer patients are at a greater risk of admission to hospital for cardiac events or bone fractures. Those undergoing ADT have a further increased risk. Women undergoing hormone therapy for breast cancer are often prescribed bisphosphonates to protect against fractures and this practice needs to be extended to men being treated with ADT. Awareness of the high risk of cardiac events should be raised to prompt discussion of lifestyle changes to reduce risk.
Using clinical attendance patterns to determine likely survivorship journey (colorectal cancer, multiple myeloma, hodgkin’s disease) in England
James Wells Monitor Group, Europe
James was challenged with studying the route from diagnosis and defining the same from both the healthcare and patient perspective.
Electronic Patient reported Outcomes from Cancer Survivors (ePOCS): preliminary results from feasibility testing of a scalable electronic system for collecting pros and linking with cancer registry data
Laura Ashley, University of Leeds
The ePOCS study aims to test the feasibility of an electronic system for regularly collecting patient reported outcomes (PROs) and linking these with Cancer Registry data.
The premise of ePOCS is that this will increase and improve the patient experience. More information can be found via the ePOCS website
~~~~~~~~~~~~~~~~
Findings from a National Audit of Cancer Diagnosis in Primary Care in England
Greg Rubin, Medicine and Health, Durham University and Sean McPhail, NCIN
A national audit of cancer diagnosis in primary care was undertaken in 2009/2010 as part of the NAEDI (National Awareness and Early Diagnosis Initiative) and address perceived deficiencies primary health care performance in cancer diagnosis. 17 of the 28 cancer networks in England took part. 3 networks used a sampling approach to practice selection. In the remaining 14 networks all practices wishing to participate were able to do so.
Data was collected on 18,113 patients by over 1,000 practices in 17 cancer networks.
Data quality was high in most categorical fields including stage and considered 90% complete.
Comparison was made with the cancer registry data and showed that the dataset was representative.
1,066 (5.9%) of patients were described as housebound
934 (5.2%) had a communication difficulty.
Both disabilities were associated with significantly increased odds of later stage at diagnosis while age, sex and ethnicity were not.
The median duration of the primary care and referral intervals was 4 days and 12 days respectively, with considerable variation by cancer site. Emergency presentation, usually associated with worse outcomes, occurred in 12.8% of all cases but ranged from 3.8% (breast) and 40.0% (brain). In 6.1% of cases the GP believed that better access to investigations would have reduced delay in diagnosis. This also varied considerably by site, rising to 19.5% for brain and 12-14% for ovary, pancreas and kidney.
In conclusion this report showed that the analysis method was effective however as we know we need more awareness at a GP level to reduce late diagnosis. Increasing the use of this data capture and evidencing this back to GPs will aid in improvement at this level.
One other piece of information that came from the report was that there was a big disparity between primary and secondary cancer referrals. Secondary being
~~~~~~~~~~~~~~~~
Variations in usage of the two week wait referral system in general practice
Carolynn Gildea, Trent Cancer Registry and David Meechan, Trent Cancer Registry
Carolynn and David had been asked to investigate the patterns in the use of the two week wait referral system by GPS. Knowing that early diagnosis is an important part of the cancer outcomes strategy and within this, the two week wait referral system plays a key role.
They looked at three measures to do the study: referral rate (no of 2 week wait referrals as a standardised rate); conversion rate (proportion of 2 week wait referrals resulting in cancer diagnosis); detection rate (proportion of cancers referred through the two week wait system); and then analyse and understand the data in comparison.
The results showed significant differences in the way GP practices use the two week wait referral system for the diagnosis of cancer. Relationships between the three measures demonstrate complex patterns in practice referrals; as expected, increases in referral rate correspond to decreases in conversion rates and increases in detection rates. However, surprisingly, conversion and detection rates appear to be positively correlated.
However it was also pointed out that approximately 25% of people with cancer don’t have cancer waiting time records recorded! This may be due to a number of different reasons; bad recording; rare cancers being recorded as a simple alternative; or missed data.
It was also thought that this report, and ongoing reporting, could be used to identify trends in GP practices, particular practices of individual GPs within a practice and then any training/support/advice that needs to be addressed at a GP practice level as well as a higher level in regard to commissioning.
One other statistic that stuck out for me from this presentation… 23% of cancer cases are diagnosed via Accident & Emergency and 24% of cancer cases are diagnosed via GP. Surely GP percentage should be much much bigger?
~~~~~~~~~~~~~~~~
Plenary Session: Thames Cancer Registry at 50 years
In celebration of the first 50 years of Thames Cancer Registry, there has been a report prepared, also online, that is a really valuable source of information and data.
We also saw a film that was made by a couple of the employees about the history of Thames Cancer Registry.
Worth a look to understand that data has been collected for the last 50 years, how the ideas and planning that was put in place all those years ago still stands proving the forward thinking of the TCR.
Maggie Barker, Medical Director and also Henrik Moller presented some of the report details and story behind TCR. Followed later by a fun presentation by Dick Skeet with memories of the TCR (he’s featured in the film!).
~~~~~~~~~~~~~~~~
Hormone receptor status and ethnicity in women with breast cancer in North East London
Ruth H Jack, Thames Cancer Registry
Ruth presented from data in NE London with a Breast Cancer diagnosis between 2005-2007. 2,417 women were diagnosed. 128 of them were diagnosed with triple negative form of breast cancer.
Her data also showed that TNBC was more likely in younger women. Also there was an increase in deprived areas.
Ruth spoke about more information being needed and research in this area with a particular focus on obtaining relevant data from all the ethnic groups.
~~~~~~~~~~~~~~~~
DAY 3
Plenary Session: Supporting Commissioning
Chair – Professor Sir Mike Richards, National Cancer Director for England
Commissioning in the new NHS
Stephen Parsons, Director, National Cancer Action Team
Stephen spoke of our wishes to commission cancer services that are the best in the world. We must achieve this and are moving toward it however aware that we have a long way to go. He did acknowledge the wonderful work that has been presented at the conference in collating and managing data so that we can utilise these tools to improve cancer services so that we not only lead the way but excel in our services.
Effective commissioning: There are concerns that there may be variability and quality of commissioning between areas however he believes that by providing and learning from information available to us even today in the data sets collected, and ensuring data, reporting and information is of a high quality, we can achieve effective commissioning.
The move toward information being in one central place is driving the views toward better outcomes.
He spoke of a Commissioning support pack for all, which will including information which MUST be informing, engaging, empowering and timely.
The information to be collated should include the incidence of cancer; prevalence and survival; different aspects and outcomes; and to share information such as expenditure and variation between the PCTs as they stand now.
There should also always be comparisons made with regard to cost effective treatments. Not only the price of a treatment but the effectiveness of using that treatment over another ie looking at survival and outcomes too.
He also spoke of GP consortia to be made up of Clinical Commissioning groups which in turn are made up of a variety of health professionals not just GPs.
Also Clinical Senates – perhaps 15 of them across the country. These Senates will therefore cross different consortia and be able to share learnings and information and indeed to have some power in ‘bulk buying’!
The question was asked one more time about patient involvement in commissioning. Stephen advised that it was his understanding that patient/users will be involved in both the Clinical Commissioning Groups and the Clinical Senate levels.
The questions that NCAT have posed about commissioning:
What are the key facts/issues that commissioners should know?
What do they feel is most important?
There are a number of myths that need to be dispelled surrounding commissioning.
Key messages that need to be put across to the GP consortia (and understood!)
- incidence of cancer is rising
- people are dying unnecessarily
- want to save 5,000 lives from cancer but in order to excel we should be saving more than 10,000
- late diagnosis is a major factor underlying bad survival rates
- 6% of NHS budget is still being allocated to cancer services – this percentage has been the same for many years (whilst other budgets are being cut, cancer services remains at 6%)
- Not all cancer interventions are expensive
How to support commissioners
- save lives
- improve quality of life and care – patient experience
- optimal value for money
Saving Lives
- Public awareness, early presentation; early diagnosis
- Supporting GPs to investigate and refer
- GPs to have more diagnostic equipment together with training and information
Improve quality of life and care – patient experience
- Prevent unnecessary hospital admissions
- Reduce length of stay in hospital
- Improve access to Cancer Nurse Specialists
- Patient information prescriptions and training on how to use them for health professionals, information officers and the public
Optimal value for money
- Invest in early diagnosis
- Reduce emergency admissions
- Enhanced recovery programmes and self-management
Benchmarking information – utilising data and reports so that there are service profiles upon which GP commissioners can make changes, learn from etc
Conclusion
Primary focus of all NHS funded care to provide high quality care and improved outcomes.
Commission and deliver cancer services that match best in the world
The Challenges ahead are significant but the prize is greater!
~~~~~~~~~~~~~~~~
Cost of skin cancer in England, including projection to 2020
Dr Julia Verne, South West Public Health Observatory
Julia described how difficult it was to obtain good data with regard to skin care and melanoma. The main reason for this is that often GPs will deal with the removal of moles or skin tags etc and these won’t necessarily be recorded correctly. GPs and local health care professionals are being encouraged to record this data more effectively.
However one thing that was plainly obvious… skin cancer is on the rise in the UK. More work has to be done in the awareness arena to ensure that people in the UK are aware of the dangers of using a sunbed but also tanning without any sun protection.
The best place for information is www.swpho.nhs.uk/skincancerhub which provides information about awareness campaigns, symptom checker, skin cancer profiles in the UK etc. Worth a look and perhaps this is something you can share with local groups such as school and colleges in your area.
~~~~~~~~~~~~~~~~
Variation of surgical resection for lung cancer in relation to survival: population-based study in England 2004-2006
Professor Henrik Moller, Thames Cancer Registry
Henrik presented information and statistics regarding survival following surgery for lung cancer. The full report is available on the Thames Cancer Registry site.
~~~~~~~~~~~~~~~~
Plenary Session: Early detection
Chair – Sara Hiom, Director of Health Information and Cancer Data, Cancer Research UK
Cancer Intelligence – a vision for the future
Professor Sir Mike Richards, National Cancer Director for England
- completeness and timeliness
- staging, only 40% of this is recorded. We should be achieving at least 70%
- pathology reporting is variable or poor. There needs to be more standards and better/clearer reporting
- Imaging. Again this varies and needs to be clearer and more standards adhered to
- Chemotherapy. This data is not yet being collated at a national level – 100% of this need to be collated nationally
- We’re only just linking our data with primary care units and not in all locations. This needs to improve significantly and also data to be more standardised as well as clear and complete.
There is little known or reported about
- comorbidity
- late affects
- quality of life
- recurrences/secondaries/metasteses
“There is an increased demand on complete and timely intelligence”
Cancer is leading in the information revolution in health but still can be improved”
~~~~~~~~~~~~~~~~
Promoting early symptomatic presentation of breast cancer: implementing an evidence-based intervention in routine clinical practice
Dr Lindsay Forbes, King’s College London
Lindsay reconfirmed what we should all know, earlier diagnosis of breast cancer (like all cancers) is a key factor in our survival rates. The need to promote early symptomatic presentation is something we should all be participating in. How can we do that?
- screening programmes
- earlier referral to diagnostic tests
- awareness of cancer and encourage earlier presentation
Health professionals delivering interventions to promote early presentation for breast cancer in older women.
20-30% of women delay presentation >3 months (1999)
there is a clear link between delay in diagnosis and survival for breast cancer (1999)
2/3 of women present symptomatically
>500 breast cancer deaths per year for women presenting >3 months
Older women think their risk of breast cancer is lower – wrong! The risk increases with age. We should encourage older women to go for their regular mammograms – so many skip appointments with the thought that they don’t need them and their risk is lower!
~~~~~~~~~~~~~~~~
Additional sites and sources of information:
edric (Fighting cancer with information)
ukacr – UK association of cancer registries