As a patient advocate I often get asked to attend conferences and meetings. Part of my role as a patient advocate is to share my learnings both as a patient and subsequent to treatment. The piece that is invaluable to organisations is that patients can work independently of any charity or company mandate. By this I mean we are able to speak our minds and say what we think or what we have learnt without needing to be loyal to the green of Macmillan or Pink of Breast Cancer or Yellow of Sarcoma.
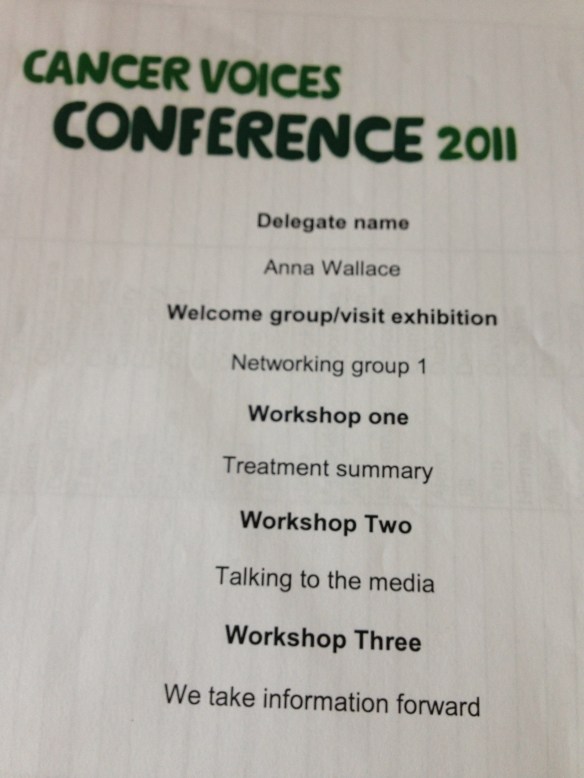
Macmillan Voices are a scheme set up for patients and carers to have a ‘voice’ within Macmillan and help shape future services by their involvement. It is often by way of focus groups on particular subjects (I’ve done many of these for them) or by completing surveys or reviewing leaflets and documents before publication. The Macmillan Voices Conference is an annual event where the Voices get the chance to get together. Throughout the 2-day conference there are workshops and networking groups.
There is clearly a great deal of investment from Macmillan in the Conference and I truly hope that the work we, the Voices, are doing during the Conference is used effectively. I’m acutely aware that this is funded by people’s hard earned money donated via some fundraising event.
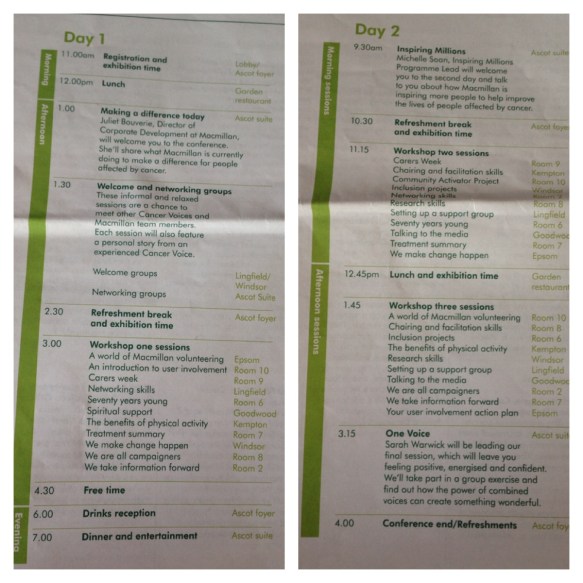
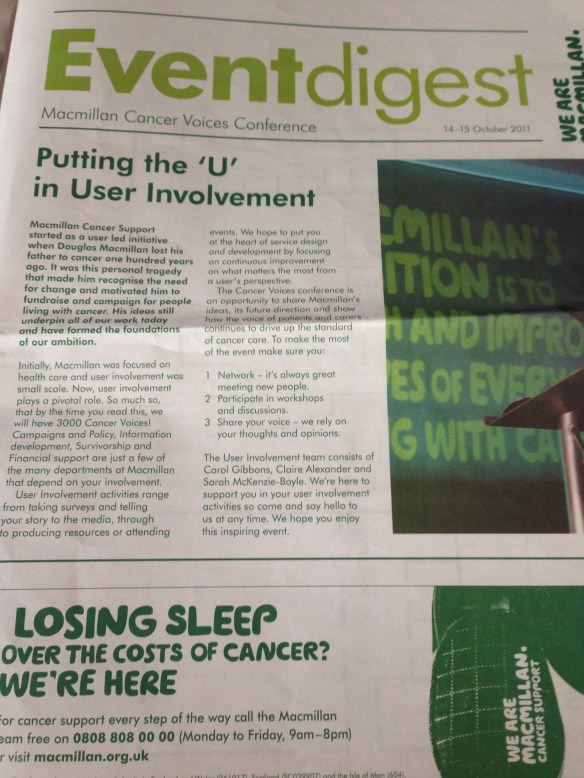 Our Conference Newspaper/Programme
Our Conference Newspaper/Programme
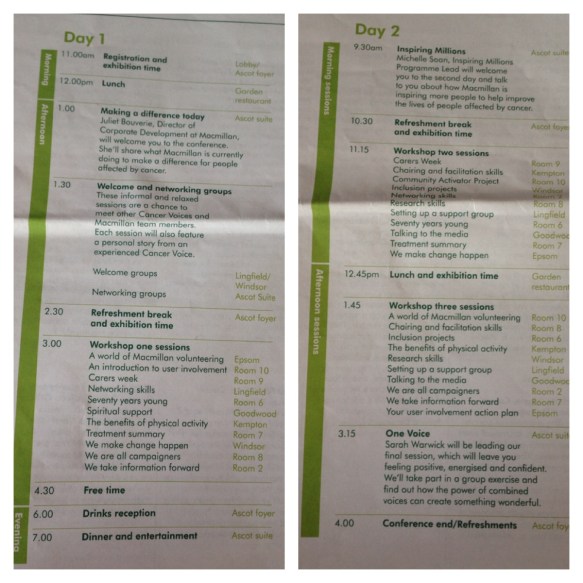 We are welcomed to the Conference during the opening plenary by Juliet Bouverie, Director of Corporate Development at Macmillan.
We are welcomed to the Conference during the opening plenary by Juliet Bouverie, Director of Corporate Development at Macmillan.
Juliet introduces herself (she’s new to the role) and tells us a little about why she’s passionate about her role in Macmillan. She also talks a great deal about the fundraising at Macmillan, some of the events that have happened and how grateful they are for all the monies raised. (Sadly to me, this came across as another plea for money and since we’ve all given up our time to be here and are Cancer Voices doing many things for Macmillan it feels insulting to ask for more!).
Juliet then gave us some facts and figures about fundraising, numbers raised, spent and people living with cancer.
This last year £137m has been raised of which £97m was spent on cancer support.
In 2030 Macmillan believe that the numbers living with cancer will be double that of today. Currently 2m people living with cancer. In 2030 they estimate 4m people living with cancer.
There is an urgency not only for a cure for cancer but to ensure there is support and assistance for those living with and beyond a diagnosis of cancer. Often the emotional and psychological aspects are overlooked in favour of the physical. All three aspects need addressing and supporting.
Juliet also spoke briefly about a Macmillan project to run training courses for all Boots pharmacists. Clearly they have a corporate deal with Boots but I’d like these courses to be offered to all pharmacists no matter which company they’re employed by. Personally I rarely see the pharmacist in a large Boots chemist but am more likely to chat to the pharmacist in a small chemist and aware that they often have more time for me too!
Networking Group
Within our first Networking group we heard a story from another Voice about her experience of surviving cancer. This led to a group discussion about survivorship and where people had found support and information. We discussed the survivorsforsurvivors website, the Cancer Survivor’s Companion book, support groups within Facebook and Twitter and of course charity-led online forums. As also discussed how to ensure that any late effects from cancer treatment, particularly from childhood cancer treatment, was also supported.
I think it’s so important that doors are left ajar for people who have gone through a cancer diagnosis at any age. Many people ‘just get on with’ cancer and then are left floundering some months/years later when they think about what they’ve experienced. Or that side affects take very different forms and are at very different times in ones life but still need addressing and supporting when they manifest themselves. There shouldn’t be a time limit on getting support.
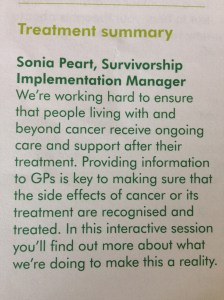
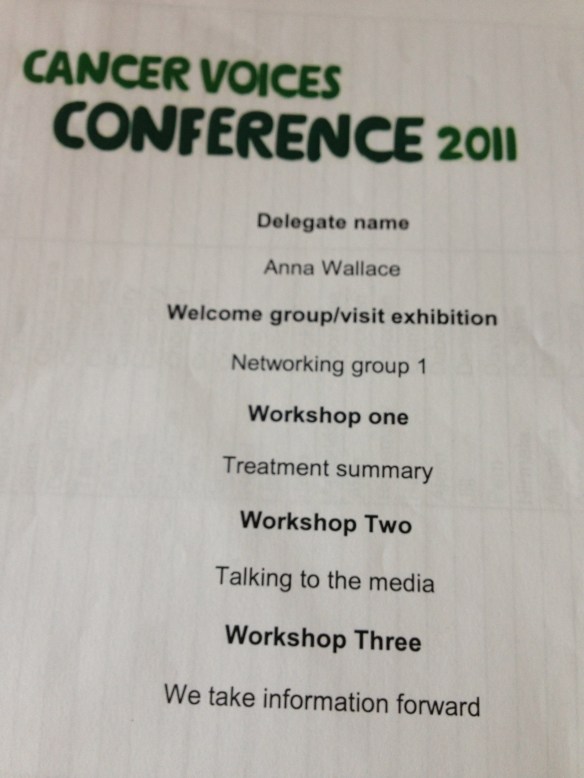
After lunch we headed off to our Workshop One sessions. I had chosen ‘Treatment Summary’.
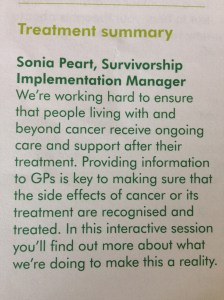 Treatment Summaries are a fascinating beast and once that has had much airtime of late. Essentially ‘Treatment Summary’ or ‘Patient Passports’ are a brief medical history of a patient’s journey with cancer. They are much like the ‘red book’ that parents were given when I was born and that documented all vaccinations, Dr visits etc until I was 16. Every parent managed to keep these books safe and take them with them on every medical visit their child made.
Treatment Summaries are a fascinating beast and once that has had much airtime of late. Essentially ‘Treatment Summary’ or ‘Patient Passports’ are a brief medical history of a patient’s journey with cancer. They are much like the ‘red book’ that parents were given when I was born and that documented all vaccinations, Dr visits etc until I was 16. Every parent managed to keep these books safe and take them with them on every medical visit their child made.
What the Treatment Summary/Patient Passport is aiming to do is to keep a full record of the medical journey in one place. As a patient I am all too familiar with having to constantly ‘remind’ or tell my history with cancer, every date and every detail. The problem with this is that I may forget some detail or having not understood the medical importance of a piece of information, have missed it out. This then leads to problems. For the old/infirm or (err) unwell this is even harder to manage. Particularly if they have different family members or carers present at different consultations.
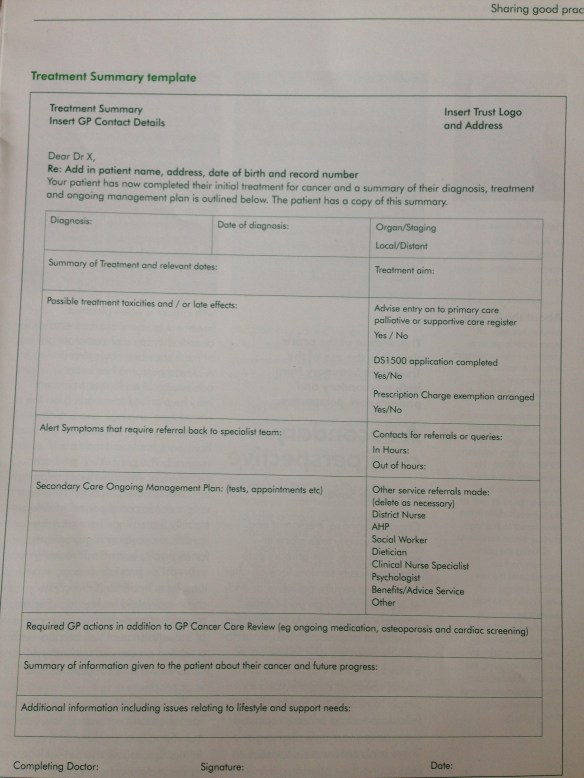
Macmillan have devised the Treatment Summary template
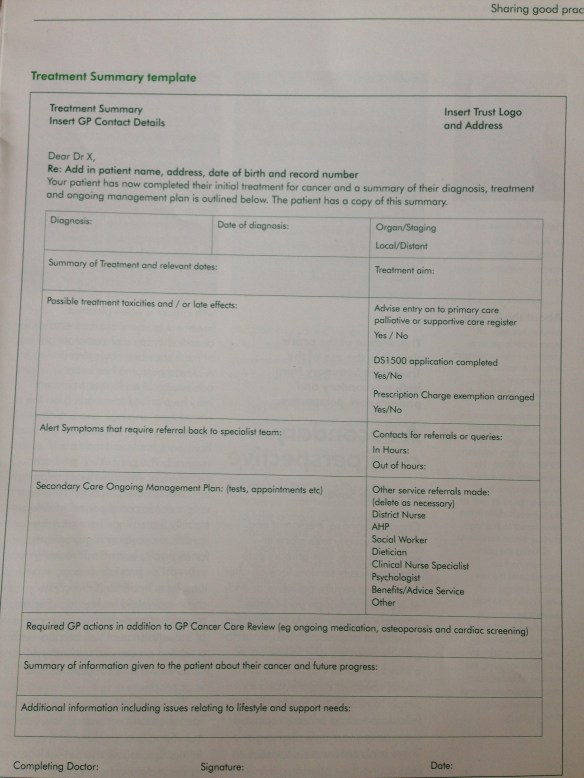
All very valuable information and is a great idea.
The barriers to this would simply be asking the medical team who are already stretched, to complete yet another form, ask them more questions and then to organise a method to send these treatment summaries to the GP (in addition to any usual paperwork).
Another barrier may be that each Trust/Hospital/Clinician may require slightly modified forms or information. Then if the Treatment Summaries appeared in different formats at the GP office, they becoming confusing and laborious to read meaning that they may end up in a file unread.
BUT equally disappointing was that Macmillan (Juliet Bouverie was present in this workshop) appeared to be completely unaware of the other organisations, charities and hospitals that had been working on their own Treatment Summaries. We have been discussing it on committees that I’m involved with at the Royal Marsden, NW London Cancer Network, SW London Cancer Network, C&W LinK for quite some time and I’ve seen the results of other people’s work.
The Patient Passport (very similar to the Treatment Summary) is now live and working well for many. There are ones by Royal Marsden, Chelsea & Westminster, West Middlesex, East Cheshire, NWLondon/Imperial and many more. Some of these are ‘advertised’ as being required for vulnerable patients but can and are used for many more than just the ‘vulnerable. There are also private companies who sell ‘Patient Passports’ allowing the patient to keep a summary of all their treatment records and to take these with them to any medical appointment. Much like our parents did when we were children. Juliet seemed genuinely surprised that anyone else had thought of the idea of Treatment Summaries and promised to investigate.
I’ve heard the argument that we would lose our patient passports. How many parents lost their red books?
The difference between a Patient Passport -v- a Treatment Summary is that the patient/carer is responsible for their own information. This is in addition to the information shared between health organisations in the ‘normal way’ but adds another level of information easily accessible and digestible that the patient/carer can produce at every medical appointment… and update at the appointment too.
What frustrated me about today’s workshop was the complete lack of awareness of any other organisation or NHS Trust work in this area. Macmillan have spent, I’m sure, a great deal of money on this project without consultation with others. As it is there are perhaps already too many Treatment Summaries out there. A GP in West London could well get sent 4 different types from the list of those already published. How on earth are they meant to know the differences on each? Most urban GPs will have 6,000 patients in their practice of which approximately 200 will be living with cancer.
Dinner
In the evening of the first day of Conference there is a dinner to which all attendees are invited. Always a good opportunity to meet new people and catch up with some old faces too.
———-
Day 2
———-
Our day begins in the main hall with a presentation by Michelle Soan, Inspiring Millions Programme Lead. She spoke to us about a new project called ‘Inspiring Millions’ as a way that we can spread the word about Macmillan and the reasons everyone should be inspired to fundraise for Macmillan. I can’t help but feel that since we’re all Voices attending the Conference the ‘hard sell’ is overkill but hey ho! Here’s their video explaining Inspiring Millions.
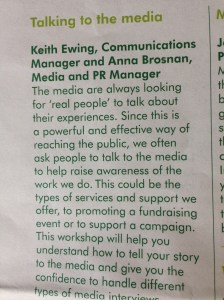
Workshop Two – Talking to the Media
This workshop was aimed at those of us who are often asked to talk about our experience, particularly with reference to the TV, newspapers and radio. Many people in the workshop were able to share their own experiences of working with the media. For many it went well but for others they explained what had happened when they had been put on the back foot or perhaps hadn’t been briefed about the discussion properly. Many also spoke of the emotional aspect to share your story. It’s wonderful for others to hear and understand they are not alone in their own diagnosis but there’s a warning that often bringing up your own story brings with it memories or feelings that you’ve long since buried.
Some hints and tips from this workshop:
- Media is often very reactive to what’s happening in the world. Therefore you may be asked to participate with little or no notice. Always be prepared.
- Some TV/radio can be pre-recorded and edited. Be aware that punchy shorter statements are more likely to make it into the final version and not on the cutting room floor. Therefore word your important messages well.. and briefly.
- Always ask, when first contacted, if the piece will be live or recorded. If live, how long will you have to speak. Prepare accordingly.
- If your being asked to be interviewed for a written piece, ask to read it before it goes live in case of any inaccuracies.
- Ask what sort of questions you may be asked and if there are any you can see before the interview.
- Ask for a copy of the finished film, feature, interview or piece. It’s not always possible but if you can retain a copy for yourself, it will be useful.
- You don’t have to be an expert on the issue at hand but rely on your experiences and signpost to experts you are aware of such as Macmillan.
- Its useful to have 3 key things you want to get across during the interview. Then if you get stuck with a question you can guide it to one of these points.
- Have some water to hand so you don’t get dry throat.
- During filmed interviews always look at the reporter not the camera.
- Be aware that you may feel you have been cut short during a live interview. This is because of time restrictions not something you’ve said.
- Try to smile a little. Even on the phone or radio you can ‘hear’ a smile.
- Take a deep breath and relax.
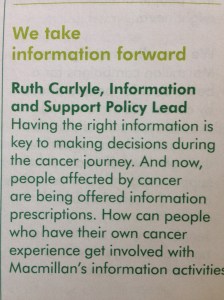
Workshop Three – We take information forward
 This workshop related to a number of information resources:
This workshop related to a number of information resources:
Promoting Information Prescriptions – This system that was created and started by NCAT. You may recall that I spoke of my involvement as a patient reviewer here. My mention of it from the NCIN conference and my speaking at the recent Learn and Share event.
So this was where the project had got to… Macmillan had taken it over. No wonder why the wonderful reviewer system had broken down. How incredibly sad that NCAT had a host of trained volunteers who were ready willing and able to review, write and process the information quickly and efficiently. So that many information pathways can be put into the system and accessible to people needing it at a time when they need it. Why on earth wasn’t this aspect of the project taken forward and at the very least these trained volunteers asked if they’d like to continue the project for Macmillan instead of NCAT?
During the workshop we have a walkthrough of the system and I’m astounded at the level of basic information there now is for cancer. It all appears generic and I know that there is little hope of getting any information about any rare cancers or support for them from the system. Have a look here.
Getting involved in Information & Support Services – Macmillan run over 140 cancer information and support services across the UK. In hospitals, libraries, community centres and hospices. The services offered range from information about specific cancers, treatment options, signposting to relevant clinical, social care or obtaining travel insurance, understanding the information or simply having time to talk. Each centre is run by a team of people including an Information Specialist and trained volunteers. Cancer Voices are encouraged to volunteer.
Getting Involved in reviewing books – Macmillan use reviews by people affected by cancer to help compile a list of suggested books for use in public libraries and information centres. Reviews are also added to Macmillan Cancer Support website. A link to a review of the wonderful Lisa Lynch’s book ‘The C-Word’ here. Cancer Voices regularly get asked to review books.
Promoting core book list in libraries – Macmillan have put together a list of core books that are recommended to librarians about cancer. This list should allow them to make informed judgements about which books to stock, how to select and appropriate range of materials and when to replace books. This guide will also enable to librarians to recommend specific books when asked by the general public. Cancer Voices are being urged to get involved by working with Macmillan to contact libraries local to them.
The Conference closed with a session entitled ‘One Voice’. The programme said this would leave us “feeling positive, energised and confident.” Sarah Warwick who hosted this session asked the group to stand, dance, move and sing. An interesting ask and very isolating for those that were in wheelchairs, crutches or unable to move easily. Even harder for those with a tracheostomy. As I watched the group of attendees cautiously attempt to follow the instructions, I also noted a trail of people heading for the door and home. I shortly followed them out. Furious on behalf of all those who ended a two day conference where they had volunteered their time, energy and commitment to Macmillan to leave feeling humiliated that they couldn’t participate in the closing session. I’m quite sure, like me, they didn’t leave feeling any kind of positive, energised or confident.