Dr Rachel Brindley (Clinical Psychologist) and Elaine Stewart (Cancer Support Specialist), London Maggie’s Cancer Centre
Morning Talk – What to do when treatment comes to an end? – Practical, emotional and psychological issues
What’s it like to be facing this diagnosis in your country?
What are the challenges?
- Majority of people say they weren’t offered support. But the search for information helped however it was their way of coping which might not be right for others.
- Misunderstanding of what palliative and hospice care is. Perhaps the communication isn’t good enough to understand what options are. Discussions between Patient and Dr need to be better to understand the options but also to think about what is the job of an oncologist, palliative care, hospice etc. Learning a new language.
What are the supports?
What are the main psychological issues that people with advanced disease face?
- Living with uncertainty. Realise the disease is progressing and recurrences but not knowing and living along side the disease whilst maintaining a quality of life.
- Significant adjustment process that needs supporting. Adjusting to the knowledge of advanced disease but finding your new place.
- Fear of future of family if I die?
Ripple effect of cancer:
Medical – treatment effects, nutritional needs, physical
Quality of life – Sleep, leisure activity, shopping, socialising (eg meals)
Relationships – Changing roles, sexuality…
Difficult emotions – Low mood, anxiety, guilt, shame, anger (at disease, at family at God)
Self Image – Body image, self-esteem, confidence
Existential–Spiritual – Meaning of life, create a legacy, purpose…
Financial/Legal – Work status, holiday insurance…
Q – Psychological support to the physicians?
A – It’s also a burden on the clinicians and medical team. Is this why they’re not best to share bad news.
Fears and questions about death and dying?
What are some of the fears?
What do people want to know?
What is it like talking about these?
Can be victims of complementary and alternative therapy?
Italian Dr shared a story – Shocked on his very first day of work in new role in LA, he was taken into patient’s room. Colleague starts talking.. in next few hours/days explains respiratory and cardiac arrest is near. We can resuscitate and will only delay a few days. Shocked about how brutal they were with the patient.
In Italy the percentage of patients with this kind of information is only 1% or less that are given details about death and dying. In Italy many patients don’t want to know they are going to die. Physicians problems start much earlier than this point.
Very individual choice about knowing what is going on.. time to clear things, discuss with relatives, friends etc think about funeral and future of family.
Patient choice… has to be a sensitive and individual choice by patient.
When do you discuss?
Again very individual to find the time to discuss. Discuss in part. Listen to learn what the other person needs to hear.
Fears about death and dying
Fears about dying:
1. Fear of the process of dying
2. Fear of the consequences of death for loved ones
3. Existential fear of death itself
Planning Ahead
What does this mean to you?
What would be helpful for you to think about?
What resources are available to help you to plan ahead?
- Comment from member of the audience: for many in the UK we have never experienced death in the first 40 or so years of our life. Death isn’t talked about.
- Comment from another member of the audience: – Clinician discussions are often very different and difficult. Training for clinicians and learning to signpost and be honest to refer.
Stages of Grief – Kubler-Ross
Denial -> Anger -> Bargaining -> (Anxiety) -> Depression -> Acceptance
Not a case of working through but cycling back. Perhaps anxiety is missing on the diagram?
Perhaps should be ‘Not knowing’ at the beginning of diagram.
Some people may never get to the Acceptance phase but back and forth earlier on –ie they’re not able to accept death.
Perhaps include Guilt
Self-Care
Close involvement with people at end of life involves managing complex medical problems and working with high levels of emotional distress
Discussion
Consider the impact that working with people with advanced disease may have on you and other professionals.
1. What signs would you want to be alerted to in
a. Yourself?
b. Others?
2. What strategies do you feel would be helpful/important in preventing and managing these?
“The heart must first pump blood to itself” – S.L. Shapiro
Support staff teams
Opportunities to debrief and reflect after difficult/distressing incidents
Opportunities to discuss what went well
Peer or individual supervision
Access to training, appropriate information
Time – to reflect on work, and for own needs
Feedback from senior management: positive, constructive
Balance between work and home life.
How might you be able to carry on some of these conversations/ideas when you get home?
~~~~~~~~~~
ADVOCACY MARKET PLACE SESSIONS
~~~~~~~~~~
Barbara Dore. Chair, Gist Support UK, SPAEN
How to Organise Patient Group Meetings
Think about and objectives for patient meeting.
Objectives
- Information/Education
- Exchange between patients
- Support (you are not alone)
- Patient empowerment
- Relationships with
- Experts who may speak at meetings
- Industry experts.
- If near clinic/training/university then perhaps invite team/students etc.
- Reasons to donate (not just in terms of money. Can also be their time).
- Finding volunteers
Session formats
- Lecture presentation
- Workshops
- Case studies
- Panel discussions
- New experiences (yoga…)
- Background sessions psychological support etc)
- Vary the pace of the meeting during the day/meeting
- No more than 2 hours without a break.
- Networking time!
Topics/Speakers
- Consider the audience
- Previous feedback
- Newcomers/experienced
- Variety of subjects – from the academic, technical and practical
- Structure the day – after lunch spot needs interactive and care in planning.
- Interaction keeps the audience engaged.
- Brief the speaker as to content
- Ask them if they want time cues
- Reminder 1 week beforehand
- Prepare some questions for Q&A
- Write and thank speakers afterwards
Location
- Budget
- Site visit
- Accessibility
- Travel easy?
- Disabled access
- Car parking?
- Layout – flow
- Resources
- A/v
- Poster display
- Flip charts
- Registration desk.
- Signposting to meeting
- Refreshments (every 2-2.5hrs)
- Networking
Volunteers
Staff during the meeting
- Registration Desk
- Assistance to guests
- Passing microphones around
- Collecting evaluation form
- Taking note from the meeting report
- Distributing papers (Agenda etc)
- Photographing
- Getting Contact details
- Circulating and meetings/ welcoming all participants
- Getting photograph permission
Announcing the meeting
- Inform and invite all attendees
- Experts physicians nurses clinic
- Invitation letters/leaflets posters
- Invite by Email postal delivery, Facebook, twitter, website, email group
- Press
- Online calendar
- Continuity slides. Welcoming slide before presentation and also slide for lunch or welcome back to the afternoon session.
The Day
- Meet and Greet
- Network in Breaks
- Feedback?
- Think about next time.
Enjoy
~~~~~~~~~~
Roger Wilson and Claire Kelleher, Sarcoma UK
Patient Group Survey
Why do we do questionnaires?
- need to get information
- need to get opinions
- experiences
- often get new ideas
Need to be quite clear about objectives for survey.
Sarcoma UK is a patient led organisation. Likes to involve patients in any initiative and involvement. Part of Information Standard process is you must involve target participants ie patients. Done by various means, feedback or through email, telephone, speak to people at support groups etc.
Clear objectives in mind when thinking about questionnaire.
Who do you want to contact? Patients? Carers
- How will you contact them?
- How are you going to find them?
- How will they respond?
- How will you record numbers in a meeting and is there any value?
- Do you need documented or formal responses?
Once you’ve got data from responses what will you do with those replies? Putting the data from the questionnaire into a spreadsheet for analysis is time-consuming.
- How will you handle their replies and analyse the responses?
- Once you have an analysis what are you going to do with it?
Got to have these things sorted in your mind before you start the survey process. Otherwise it may be past its use by date by the time you use the analysis.
Claire – How we’ve used our surveys. At British Sarcoma Group Conference in February we asked specifically about written information.
Asked the group in workshop (patients, clinicians and CNSs) what they thought of information (using Macmillan and Cancer Research UK’s written info). Most people said too complex and difficult to understand ie the lesson learnt use simplest terms that we can.
Negative feedback re glossaries – most people in the workshops found it difficult to flit back to glossary rather than explaining what a word means as they go along.
Survey about information and support – what info have you found? When did you receive it? Etc… so Sarcoma UK can understand what patients are experiencing and better support patients as they should be.
Collate research data. One reason why survey used?
Use methodologies and tools that have been validated academically. So that the data can be taken seriously by professional bodies (wherever possible).
One of the tools that is most readily available is the EQ5D which looks at quality of life.
Is this form truly useful for cancer/sarcoma patients?
Currently working with Royal Marsden for sarcoma patients with advanced cancer.
Claire – Example of how patients’ information can be used within gynae-sarcomas.
There is a gap of information around this type of sarcoma.
People upon diagnosis not given information… there is very little.
Sarcoma UK are developing a booklet.
They have an information review panel (both patient review panel and a professional review panel).
All information goes through the process first with the professional panel looking for inaccuracies.
Next to the patient review panel – is it easy to understand? Is it the information they want to see?
One problem we had is that there isn’t that many people we have on the information review panel with this type of sarcoma.
We put a call out to the women we knew about to invite them to be involved in the review panel.
In January we’re holding a Webinar (with Maggies) to offer information and advice to ladies with gynae-sarcomas and also to gather information about what they would like to include in the information leaflet.
The information leaflet is then due to be published early next year and will be available on the Sarcoma UK website to download.
We do get it wrong as well…

80 responses.
People had written all over the form and written on the back of the form. Realised they were only scratching the surface with this survey. Didn’t look at it well enough or in depth.
Hadn’t expected to also see hospital doctors lack of sarcoma information as well as GP (which had been expected).
If we’d been able to test the survey with 10 or 12 patients beforehand, Roger thinks a very different survey would have gone out.
Ended up writing a three page analysis of this survey which frankly was a load of waffle as the real conclusions had no data to support them as it was supplied anecdotally in the margins of the form rather than as answers to not very well worded questions.
Lesson – get objectives right before you start and test the questions to ensure you are asking the right questions in the right way to the right people.
Q – how would you deal with when a patient asks for privacy in answering a questionnaire.
A – Responses are anonymous. Don’t ask for other personal information that might identify someone.
If someone doesn’t want to give information… they don’t have to.
~~~~~~~~~~
Ian Judson, The Royal Marsden Hospital UK
Marco Fiore, Istituto Nazionale Tumori Milan, Italy
Strategies for Metastasis in Sarcomas and Gist – Perspective of oncologist and surgeon
50% of people diagnosed with sarcoma will NEVER have another problem after primary treatment.
~~~~~~~~~~
Ian Judson – Sarcoma Unit, Royal Marsden
Management of metastatic disease – soft tissue sarcoma and GIST
What are the roles of chemotherapy for soft tissue sarcomas?
- Palliation of advanced local or metastatic disease
- Pre-operative treatment for large tumours?
- Adjuvant chemo in large, high grade, extremity tumours?
Palliative treatment of advance disease. Crudely if you lump all sarcoma together the median survival isn’t great. Probably about a year.
We did a trial in the EORTC combination v single agent – the 62012 trial
Slight improvement in progression free survival but no significant improvement in overall survival.
How can we use this data?
- If objective is response – tumour shrinkage or remove specific symptom (pressure on nerve) then justified in using combination therapy.
- If objective is palliation, then no real value in using combination therapy… single agent treatment (consequential if needed) is probably best.
What subtypes are particularly sensitive to chemotherapy?
- Most sensitive subtypes appear to be
- Synovial sarcoma
- Myxoid/round cell liposarcoma
- Uterine leiomysosarcoma
- Other?
- But N.B. – data are sparse on individual disease outcomes.
Other effective agents. We use a combination of agents depending on the sarcoma type. But we’re dealing with small numbers and difficult to assess.
Hormone sensitive sarcomas
- Endometrial stromal sarcomas & some low grade ER/PR+ leiomyosarcomas, respond to oestrogen deprivation
- In premonopausal women GnRH agonists or oophorectomy
- In postmenopausal women – aromatase inhibitors
- We usually use letrozole
When is chemo unhelpful?
What’s the future?
Molecular biological information that we can translate into new treatment.
In part:
Some tumours, types, mutations can be difficult to treat or apply a ‘rule’.
Some progress with translocations (chromosome swapping) ie synovial sarcoma translocations
Chromosomal amplifications – ie when it copies and becomes a driver for the sarcoma.
Median survival is improving as we discover more. We have more drugs being used. Differing regimens.
Conclusion
Range of treatments available for treating metastatic sarcoma.
PHYLLODES – COULD BE SARCOMA OR CARCINOMA (hence confusion about where it sits in medical teams)
~~~~~~~~~~
Marco Fiore, Instituto Nazionale Tumori Milan, Italy
Strategies for metastases in Sarcomas and GIST – A surgeon’s perspective
Looking at surgeries about how we run trials.
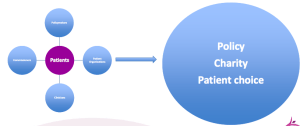
Conclusion should perhaps be that it is about patient choice and perhaps the studies should be addressed retrospectively in order to obtain patient randomisation. Patient choice needs to be made with sufficient information to make an informed choice.
~~~~~~~~~~
AFTERNOON SESSION – SARCOMA TRACK
~~~~~~~~~~
Jean Yves Blay, Centre Leon Barard Lyon, France
Update on new and ongoing trials
There are many clinical trials….
- You understood for clinical trials that we are dealing with a very well structured setting. The majority of trials are done in multiple continents.
- We are moving from a situation doing trials in all sarcoma sub-sets to a situation where we are targeting histologies. This is changing the landscape an adds a level of complexity. The end of the story will be not only focusing on sub-types but molecular sub-types within. Results in small number of patients and work collectively globally. It will not be possible to demonstrate the use of an agent
3 messages
- Global approach
- Histology Driven
- Very important in know randomised trials, approval of the agent and prove that something is superior to another.
Bone sarcomas
- Osteosarcoma
- OS2006
- Exploring bisphosphonates in a randomised setting
- FSG, EORTC, others
- Euramos 2? 5 years to do the first trial. What next in Euramos 2 trial?
- Country specific trials.
- Ewing
- Ewing 2012 (FP7)
- Comparing VDC/IE to VIDE (comparing US regimen to the European regimen)
- Exploring bisphosphonates
- EuroEwing trial
- Piloted by the German group.
- PoC studies in Ewing/Osteo
- Mifamurtide, linsitinib (EuroSARC WP6)
- Chrondrosarcoma
- PoC study of neoadjuvant mTOR inhibition
- Hh inhibitors (vismodegib) negative
- EuroSarc projects
- Chordoma
- Trials on mTOR, TKI (imatinib, sorafenib) completed
Soft tissue sarcomas
- Neoadjuvant
- Histology tailored treatment in EuroSARC (WP5)
Trying to address if we should give the same treatment.
- Adjuvant chemotherapy
- IRCI Uterine LMS 0 vs 4GT/4Doxo
Unsolved question in soft tissue sarcoma. This is not the standard for all patients and we do not know who will or won’t benefit.
IRCI – this was the first trial in the US.. no treatment –v- combination treatment. It’s hoped it will answer the important question on this sub-type.
- Surgery
- Prospective trial of no treatment in desmoids (FR)
Phase 2 study of no treatment. Often not mentioned. This is where desmoids are not affecting other things.
- (Neo)Adjuvant radiotherapy
- Retroperitoneal sarcoma (EuroSARC WP4) exploring in selected localisation of disease.
- Vortext tiral (UK)
- SAR01 trial (FR) no radiotherapy with wide margin
Largest clinical trials are in the advanced phase:
Advanced phase – randomised trials
First line
- Palifosfamide (closed Ziopharm sponsor)
- TRS trial (Pharammar, completed) – Needs further investigation.
- NCRI GT vs Doxo (UK) – Recruiting well – 220 out of 250 patients. ASCO 2015
- EorTC Trust Trial (closed for accrual). Exploring agent in first line setting.
- Dox +/-TH302 (ongoing, Threshold sponsor)
- IRCI EORTC/UK in HGUS High grade undifferentiated uterine sarcoma.
- Taxol+/-Bevacizumab (FR, Angiosarcoma) – Close to completion of accrual.
Only a few trials are addressing in histological sub-types.
Subsequent lines
- Trabectedine vs DTIC (JNJ, US, L-sarcomas)
- Eribuline vs DTIC (Eisai, World, L-sarcomas)
- Sunitinib vc cediranib (US NCI, ASPS)
- Regorafenib vs – 0 (FR, all comers)
- CDK4 inhibitor vs 0 in (US/World WD/DD LPS)
- MV vsPazopanib (FR, Desmoids)
- Cediranib vs BSC (UK ASPS)
Phase 1/11 trials
- Subset specific (right question?)
- Target specific (phase I/II)
- Molecular immunotherapy. Contrasting what was done in the 90s. Watch in next 2 years to see new trials of this kind.
- Passive immunotherapy. Means antibody which is labelled with a nesotope and recognised.
- Treated the driver target across histotypes
EORTC Network of Core Institutions
EORTC protocol 9010 (EudraCT number 2011-001988-52 NCT01524926)
Probably the future of what we are going to do in sarcoma.
Q&A Session
Q – Moving much more to molecular selection of patients in clinical trials. Is the pathologist going to become more important in making the selection decisions.
A – The role of the pathologist is central. This question is debated often. How do we link pathologist to molecular biologist? Research to routine is very challenging.
We need to bring up a budget wall with people talking to each other and exchanging information. Challenging not sure. If a pathologist is a real molecular biologist you’re fortunate!
~~~~~~~~~~
Short profiles of sarcoma subtypes
~~~~~~~~~~
Hans Keulen, Chordoma Foundation NL
Chordoma
Brief introduction into Chordoma and introduction to clinical trials
What is Chordoma?
- Malignant tumour arising from the bone of the skull base and spine
- It is a cancer and has a tenancy to be locally invasive and a tenancy to spread (metastasize)
- It’s origin is traced to remnants of primitive embryonal cells called the “notochord”
Demographics
- 5 % of the primary bone tumours are located in the spine
- 8% of the spinal tumours are Chordomas
- Incidence <0,7-1:1,000.000
- Grows at skull base (Clivus, 35%), sacrum (50%) other spinal (15%)
- Strikes people of all ages, most diagnosed in the 50s for sacral and 40s for other types
- More frequent in men than women.
Phylum Chordata: Subphylum vertebrata
- 550 million years ago Chordates emerged from the common ancestor
- Presence of the notochord is the most prominent feature of the Phylum Chordata
- Notochord is ectodermal and guides developed
Fate of the notochord
- The notochord is essential for the creation of the embryo
- Usually disappeared 10 weeks after gestation
- The notochord should not be there at the latest after 10 years.
- There are a lot of factors that can arrest the disappearance.
Recent discovery is that a certain gene called Brachyury (t-box gene). Essential for development. Absence is lethal.
Notochord and brachyury
Brachyury is over expressed in chordomas and many epithelial cancers.
Brachyury is expressed in chordomas but not in other bone and cartilage tumours.
Approximately 10% of chordoma patients it is familial.
Duplication of brachyrury gene has been observed in familial chrodomas.
When you inhibit brachyury in chordoma patients you will stop it growing.
Recent discovery from UCL – www.ncbi.nlm.nih.gov/pubmed/23064415
97% of chordoma patients harbor at least one allele of the common nonsynomymous SNP rs2305089 in the brachyury gene
Research is imperative.
Benign notochordal cell tumour (BNCT)
Should anything be done at this point?
Current treatment of chordoma
First line is still surgery. Piece by piece or enbloc depending on location.
Sometimes stabilisation of the spine is required.
Radiation therapy is a high dose (usually 3x dose of breast cancer) Specialised types, mostly proton beam or carbon ion.
Implications
- Prognosis for chordoma patients Is not that good.
- High rate of recurrence
- A lot of people get a lot of mutilating surgeries.
- Sacral chordoma usually in a wheelchair
- Survival rate has gone up but sometimes at a cost of added mobility.
In the past we saw only 10% of mets. However recently mets in sacral chordoma has recently been recorded that these are as high as 30%. There is doubt if this might be due to surgery not being good enough – possibly caused by seeding.
No chemotherapy
20-20% cure rate.
Survival
Median was 6.29 years
Remarks – survival is increasing to 7-9 years, but with increased morbidity from surgery and radiation.
Chordoma vs Chondrosarcoma
Mistaken on routine histology
Epithelial v Mesenchymal origin
Immunohistochemistry
Cytokeratin
Brachyruy
Survival
Much better for chrondrosarcoma (gr1)
Misdiagnosis is less common now.
Recent developments
Using Carbon Ion instead of Proton radiation particularly in sacral chordomas night even replace surgery as first line treatment (ECCO 2013)
Radiation before or during surgery offers promising results with respect to recurrence and seeding.
Increasing number of target identified for trials with existing drugs.
Other trials….. not just drugs
e.g. Carbon Ion vs Proton Beam radiation – HIT Heidelberg
Carbon Ion vs Proton Beam radiation – HIT Heidelberg
About Chordoma Foundation
We are a very small patient group. Worldwide we are less than Sarcoma UK!
Our mission is to improve, extend and ultimately save the lives of chordoma patients by:
Accelerating the development of more effective treatments
Helping patients across the world.
One in a million, on a mission – Chordoma Foundation
~~~~~~~~~~
Beatrice Seddon, UCL Hospital NHS Trust UK
Uterine Sarcoma
Gynaecological sarcomas – where are we in 2013?
Incidence of gynae sacomas
1985 – 2009 5950 gynae sarcomas diagnosed in the UK
9.2 case per million female population
285 cases diagnosed in 2009
Peak incidence 30-60 years
NCIN Gynae sarcoma report soon to be published.
Classification WHO 2003
Uterine Mesenchymal tumours *****
Smooth muscle tumours
Endometrial stromal tumours
Do not include malignant mixed Mullerian tumours
Location of tumours
85% of gynae sarcoma arise in the uterus
7% I the ovary
4% in the uterine malignancies
Sloan Kettering uterine leiomysosarcoma nomogram – overall survival probability prediction tools
Management of gynae sarcoma
Surgery – Most important component of treatment
~~~~~~~~~~
Marco Fiore
The interdisciplinary process of diagnosis in soft tissue sarcoma
MDT involved
Pathologist, medical Oncologist, thoracic surgeon
Web based National Rare tumours network, radiation oncologist
Surgical oncologist Radiologist
Sarcoma MDT
Many specialists have routine activity with MDT team.
Weekly routine meetings with the specialists, pathologic round, clinical round and MDT outpatients.
Biopsy
Any deep mass OR bigger than 5cm OR increasing in size
- Hystologic exam (better than cytologic)
- Think about possible surgical incision
- Keep high-level of clinical suspicion
- Be aware of usual misdiagnosis -> deep large ‘hematomas’ are virtually impossible if no trauma history and/or anticoagulant drugs.
Core-needle biopsy
Local clinic
Usually two samples.
Pathologist – new classifications WHO classification of soft tissue tumours
In common cancer they are white or black
Benign – no problem.
Malignant – diagnosis of cancer.
Within soft tissue transfer it is a scale of white, greys and black,
Benign, Intermediate aggressive tumour, (locally aggressive) or (rarely metastasizing) Malignant.
Different decision for soft tissue sarcoma diagnosis.
Soft tissue sarcomas can be diagnosed anywhere in the body and surgery on sites can be very varied yet the tumour type could be the same histology. Anatomic constraints.
First think the overall strategy:
- Histology specific (and grade)
- Combination of natural history
- Different sensitivity to different drugs
- Different radio-sensitivity
- Site specific
- Respectability
- Reconstruction needs
What I can do + what the tumour can do = What I should do.
Please note, overall strategy should think in advance.
Sometimes it’s important for the surgeon to consider what to do rather than rush into it… difficult as most patients want surgery immediately but caution may in fact be best for the outcome.
Pushing tumour margins Or with infiltrative margins.
External lesions it may be better (angiosarcoma photo used) to have any chemo after surgery… that way the surgeon can see exactly where they need to perform surgery.
Functional outcome is an issue. Needs planning to ensure that particularly with arms etc that reconstruction of nerves etc is also planned to provide patient with best outcome.
Cosmetic outcome can be problematic. Such as on the head and neck. Plastic surgeon should also be consulted as part of the planning.
INT – treatment criteria
Changing over time 1987-2007
- Less amputations. Decreased from the 1st to the 4th period (9% -> 3% -> 1% -> 1%)
- Concurrent chemo—radiation therapy. Preoperatively
Local recurrence was improved. Survival did not change. Functional outcome and quality of life did.
One-shot approach. You need to think in advance for this strategy.
- Re-excision: up to 50% of the cases referred to tertiary centres.
- Impact on public health costs /reimbursement criteria??
- Impact on extension of final surgery and functional outcome.
- Psychological impact on patient and family (unexpected diagnosis: whoops! – delayed diagnosis – second opinion change diagnosis in 30%)
- No prognostic impact.
Retroperitonal soft tissue sarcoma
Probability of finding via CT scan is low.
Biopsy remains the gold standard in diagnosing sarcoma!
~~~~~~~~~~
Julia Hill, Deputy National Programme Director, National Cancer Peer Review, UK
Peer review of quality of treatment, access to treatment and centres of excellence.
What is Peer Review?
- Quality assurance programme based on National Guidance and National Standards.
- For Sarcoma this wa the Improving Outcomes Guidance.
- Guidance by nature is guidance and cannot specifically be measured. Need to be benchmarked.
- It’s not a statutory function but well supported in NHS.
Development of peer review
- Developed initially around cancer services. Broadening outside of cancer.
- First reviews took place in 2001. Been through many reviews and remodelling.
- Number of independent reviews support the continuation with recommended support.
Aims of Peer Review
- Providing safe services
- Improving quality and effectiveness of care
- Improving the patient and carer experience
- Undertaking independent, fair reviews of services
- Providing development and learning for all
- Encouraging the dissemination of good practice.
Key principles of Peer Review
- Clinically led
- Consistent in delivery
- Developmental
- Focus on coordination within and across the organisation and pathway
- Peer to peer. Clinicians working in the area reviewing clinicians and teams.
- Integration with other review systems. Hopefully no duplicating information.
- User/Carer involvement.
Benefits of the Peer Review Programme
- Proven to be a catalyst for change.
- Developmental programme
- Provides director of services and information across the country
- Identify any risks in the service by visiting and bringing to the attention we can get these involved quickly
- We have a lot of clinicians involved in process (3-3,500 clinicians who review)
- Rapid sharing
- Provision of timely benchmarking data.
The Peer Review Methodology
Annual Self Assessment -> Internal Validation -> External verification -> Peer review visits.
Reviewing evidence
- Quality measures. Ask teams to provide evidence documents to keep workload minimal. We ask for doctors that the team would be using in every day… work programme, operation policy, annual report.
- Narrative report against key themes… for structure and function. What membership of teams. What’s the training. Patient pathways and clinical guidelines. Patient experience. How do get patient feedback.
- Clinical outcomes. We are moving toward looking at clinical outcomes.
Development of the measures
National guidance
Expert Groups – nurses, allied health professionals, dieticians etc and also patients.
Consultation – get together to create a set of measures for the service.
Formal consultation – for approx 3 months.
Editing – meet again and edit etc.
Publication – measures reviewed on an annual basis to take into account changes in national guidelines.
Measures for Sarcoma published in August 2011 – NCAT Manual for Cancer Services – Sarcoma Measures
Cover aspects:
- Sarcoma Advisory Group
- Trust – inc Diagnostic Clinics
- MDT – Bone and soft tissue.
What makes up a peer review visit:
Purpose:
- Provide an opportunity to meet with members of a service to determine compliance with the quality measures.
- Identify any broader issues relating to the delivery of a quality and safe service including a review of clinical indicators.
- Provide a further external check on internal quality assurance processes.
Look at the wider picture of how the team functions against how they’re delivering against clinical indicators.
Who are Reviewers?
MDT – service users, clinicians, AHPs, Managers and commissioners…
Peers are people who have been trained and working in the same discipline as the people they are reviewing.
We don’t have reviewers reviewing the trust next door but are objective of the pathways.
Selection Criteria for a Peer Review Visit
- We don’t visit all the centres but do a risk based target for the visit. Are they meeting national guidance.
- Were there any risks identified previously that have still not been involved.
- We’re asked by organisations to visit.
- Compliance against measures with lowest performance grouping… If teams are still not reaching 50% of measures then we need to go in and see what the problem is.
- Concerns regarding the Internal Validation process.
2012/13 Peer Review Visits
12 Sarcoma Advisory Groups
145 Trusts, 19 Diagnostic teams
15 MDTs
Good Practice
Generally good provision for TYA Support for this patient group nationally
Good patient involvement overall and good examples of support
Good entry into clinical trials
Immediate risks
Inadequate referral population
Below 100 patients
Serious Concerns
- Inadequate CNS provision
- Lack of attendance at the SMDT by radiology and pathology
- Lack of oncology capacity (non-surgical oncology)
- Ambiguous/fragmented pathways (retroperitoneal and site specific)
- Poor pathway/MDT governance / Data
Recurring Themes
Reiterate points before, particular issue was some Self Assessment Groups do not benefit from same support as more matter NSSGs
Clinical Outcomes
Clinical Indicators for sarcoma were introduced in April 2013:
- % patients treated in Sarcoma centres
- Caseload by Sarcoma centre
- % patients receiving surgery
- Readmission rates within 30 days of surgery
- % patients with a recorded stage.
Working with NCIN to provide service profiles for each of our teams. Ie Cancer Service Profiles for Breast cancer Comprise of demographic data, specialist team, throughput, meeting times, practice, outcomes and recovery and Patient experience.
Outcomes of Peer Review
- Confirm quality of services
- Identify shortcomings and publish
- Publish reports about quality of services
- Timely information for commissioning
- Validate information which is available to other stakeholders
My Cancer Treatment – is the website that patients can then see and compare local services and check what the results are for their local hospital etc.
Click on Find out more to see the narrative of the report.
We know that not only patients are looking at the website – commissioners are also doing so.
Sarcoma UK have prepared and posted on their website a summary of the Patient Experience Survey results
~~~~~~~
SPAEN Partnerships and Collaborations
Progress in Rare Cancer Care
Collaborations and Networks
EORTC and EURO/SARC
Winette van der Graaf, Chair EORTC STSG, Netherlands and Estelle Lecointe, SPAEN France
What drives us as a sarcoma specialist?
If you work on frequent cancers, do randomised trials. If you work on rare cancers – find friends..
What is EORTC
Exists for 50 years.
Important institute in Europe. Main aim is to collaborative academic research throughout Europe to improve the outcome for cancer patients.
There also groups that breaching these tumour groups such as elderly, quality of life, biomarkers etc
One family of sarcoma group.
Throughout Europe
Soft Tissue Bone Sarcoma Group
- Throughout Europe
- Randomised phase 2 an 3 studies
- Interesting partner for Pharma. Difficult in a rare disease to get pharma involved however with big databases they’re interested!
- Big and relevant data bases
- Gets support from EORTC,
- Platform of discussing studies in such rare disease. But also a platform of finding friends and collaborations. We are all busy with a very rare disease for which there are not so many people available.
- Collaborative spirit.
Organisation of STBSG
- Board of group, period of 9 years
- ExCo with charis of the subcommittees
- 2 group’s meeting a year
- Young investigators of the group. Welcome new members interested in doing studies in sarcoma.
Group gets a scientific audit every 3 years. So we are audited on the way we behave and want to see minutes and outcome and publications and all activities. Proud to say the last audit took place this year and we ranked very high. Always hope that you will have good advisors to make it even better.
Subcommittees
- Local treatment – radiotherapy, surgery
- Systemic treatment – chemo targeted agents
- Pathology
- Imaging. Radiologist part of design of studies.
- Quality of life since 2012
- Public relations, starting from 2013
- … pre-clinical group to look at what’s going on in other institutes (to be set up)
Collaboration with…
- National groups in France, Germany, Spain, Italy, British, etc
- Some members are members of World Sarcoma Network. Number is increasing.
- Pharmaceutical companies
- EU grants and education (this needs to be extended)
Open studies…
Very few later stage open studies at the moment. Working hard to get new studies active.
STRASS and CREATE studies.
New intiatives
Discussions about
- Osteosarcoma French Study
- Ewing sarcoma (FP7)
- Liposarcoma CDK4 inhibitor
- GIST: fist line, second line, third line
- Elderly study: cyclophospharmide/prednisolone
- Imaging studies on STRASS
World Sarcoma Network
This is a totally different institution created in 2009 by enthusiastic people in the sarcoma field. Cooperative group gathering the main reference centres to stimulate rapid clinical drug development for sarcomas.
Enable clinical studies that could not be completed by the cooperative groups or at a national and continental level. Where it needs a global level to discuss.
In Europe, in Australia Peter Mac, Ludwig Institute Australia
World Sarcoma Network the challenges
- If you have no institute location and no funding how can you organise it. Busy of thinking of a model of how to do this. We have the international rare cancer initiative.
- Very rare disease – unattractive for Pharma
- ‘Sarcoma of the year’ 2013 gynae sarcomas. If we are not more concrete what we are aiming at then for the outer world it will be a vague institute of nice people but no objective.
- Biannual meetings during ASCO and CTOS
Examples of successful collaborations
- Trials in GIST
- EORTC – Italian and Australasian Sarcoma Group Centres in the US
With the input from all of you, there will be many more studies to come…
~~~~~~~~
EuroSARC
Jean Yves Blay, Centre Leon Barard Lyon, France
European Clinical Trials in Rare Sarcomas within an integrated translational trial network
How do we get funding for collaborative working?
Each network gets funding from different parts but how do we bring these together?
Where grants from EuroSARC came together. Tools to enable this network of networks to move in the right direction.
Some times successful in some projects but other times on our own we may be unsuccessful.
We can build something on the basis of international grants.
GOAL – EuroSARC project – Academic clinical trials with a limited number of partners but inclusive for all networks and all groups.
Interaction between clinical research <-> Translational research <-> basic research
Objectives
To address major academic questions
Involve reference centres
Tod design structure and implement 9 innovative investigator driving clinical trials of different scales on a multinational level, evaluating novel
Conclusions
- An important support for Ebased on previous work
- Academic research only
- Difficulties/problems
- Adaption to the context/change of plans.
www.eurosarc.eu website
Website
1. About sarcomas
2. 2 Eurosarc project
3. Eurosarc clinical trials
4. Patient and public info
5. Utilities
6. Members section